Hypertension
Session: Hypertension
71 - Longitudinal Association of Depression PHQ-9 Scores and Blood Pressure in Adolescents
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 71
Publication Number: 71.2003
Publication Number: 71.2003
Katherine Mai, MD (she/her/hers)
Pediatric Nephrology Fellow
Cohen Children's Medical Center
Bayside, New York, United States
Presenting Author(s)
Background: Depression is known to be an independent risk factor for worse cardiovascular disease in adults; however, there is a lack of pediatric studies examining this relationship in adolescents.
Objective: To evaluate the longitudinal association between depressive symptoms measured by Patient Health Questionnaire-9 (PHQ9) scores and Blood Pressure (BP) in adolescents followed in a large ambulatory care network.
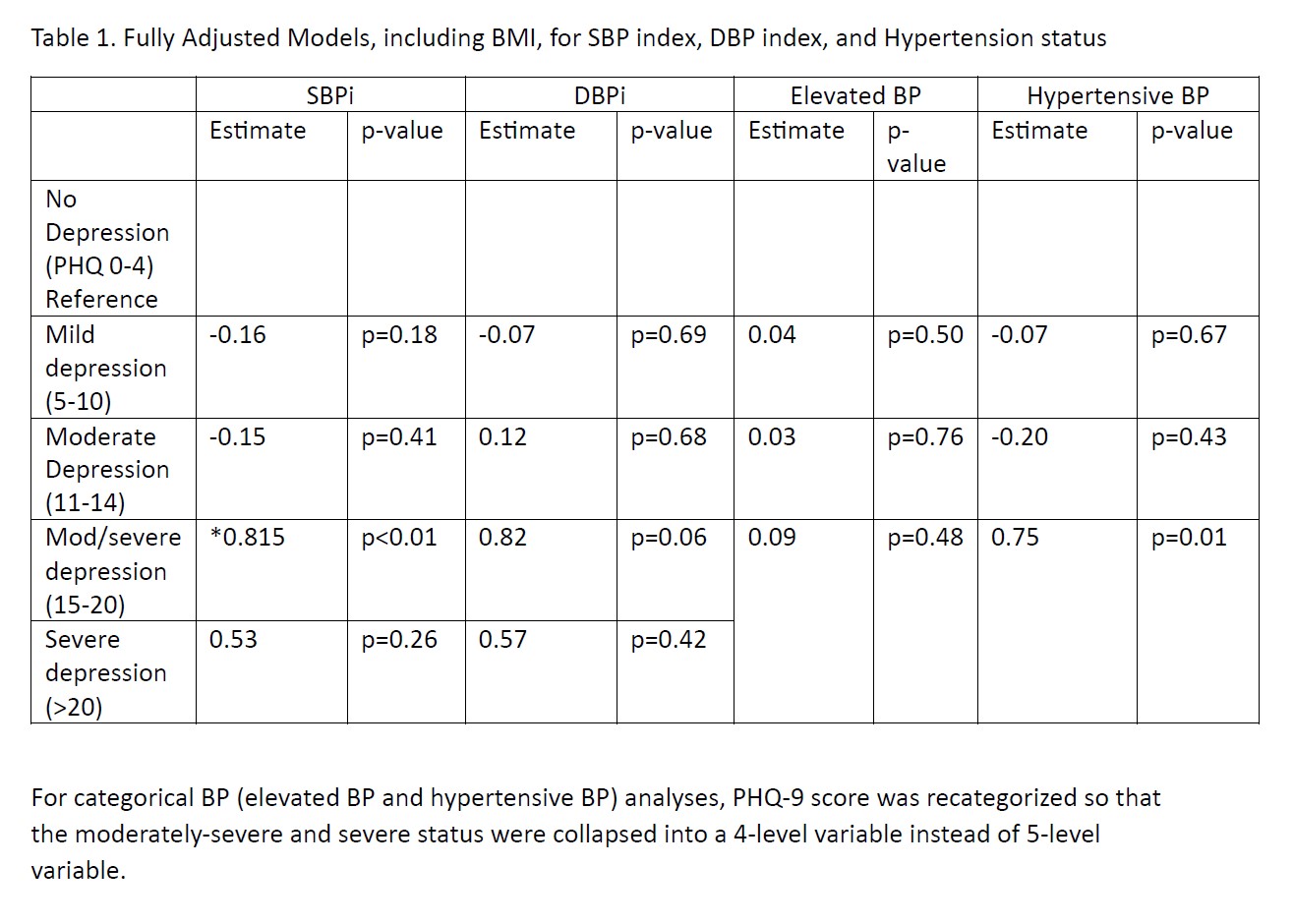
Design/Methods: The study included adolescents aged 11-17 years old who did not have hypertension at their initial visit, had a minimum of two PHQ-9 scores and two recorded BPs, and were followed at Northwell pediatric outpatient clinical sites from January 1, 2017, to May 31, 2022. Systolic and diastolic BPs (SBPi/DBPi) at each visit were indexed to the 95th percentile. SBPi or DBPi 1 indicated hypertensive BP. Linear mixed models were used to assess the relationship between PHQ 9 scores and SBPi/DBPi outcomes. Hierarchical generalized linear mixed modeling (HGLMM) was used to assess the association between categorical PHQ 9 scores and BP status (normal, elevated BP, hypertensive BP). Covariates included age, sex, race, ethnicity, season, COVID era status, and insurance, chosen a priori. BMI status was evaluated as a potential mediator.
Results: 10, 227 adolescents were included in the analysis (mean (± SD)age 14.4 ± 1.7 uears, 49.2% male, 66.6% public insurance). At the index visit, mean PHQ 9 score was 2.7± 3.9, SBPi was 0.9 ± 0.1, and DBPi was 0.8 ± 0.1. 27.4% developed elevated BP and 11.8% developed hypertensive BP at one or more time points. PHQ-9 was significantly associated with SBPi and DBPi over time after covariate adjustment without body mass index (BMI) (p < 0.001 and p=0.04, respectively). After including BMI in the model, the relationship between PHQ-9 and SBPi was partially attenuated by BMI although still was significant (p=0.01). Moderately Severe PHQ9 scores (10-15) was associated with an 0.81 increase in SBPi x100 over time, compared to No Depression (0-4) (p < 0.01). PHQ9 score was significantly associated with BP status over time (p < 0.001) but was no longer statistically significant after including BMI (p=0.18). Obese and overweight status were associated with higher SBPi and DBPi (p < 0.001).
Conclusion(s): Among adolescents in a large ambulatory care network, depressive symptoms as measured by PHQ-9 were associated with higher systolic BP over time. BMI is a potential mediator of the relationship between PHQ-9 and BP outcomes. Future research will need to be performed to establish causal inference.