Hospital Medicine
Session: Hospital Medicine 1
300 - Association of adjunctive systemic corticosteroids and clinical outcomes in children hospitalized with severe orbital infections
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 300
Publication Number: 300.363
Publication Number: 300.363

Clarelle L. Gonsalves, BSc (Hons.), MD (she/her/hers)
Pediatrics PGY-2
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Periorbital and orbital cellulitis are potentially severe infections in children and youth. The use of adjunctive systemic corticosteroid therapy has been postulated to improve outcomes by reducing inflammation, swelling, and the need for surgery. However, few studies have evaluated adjunctive systemic corticosteroid use, and no prior studies have described practice patterns in Canada.
Objective: To evaluate the association between adjunctive systemic corticosteroid use and clinical outcomes in children hospitalized with severe orbital infections, and to describe practice patterns of systemic corticosteroid use.
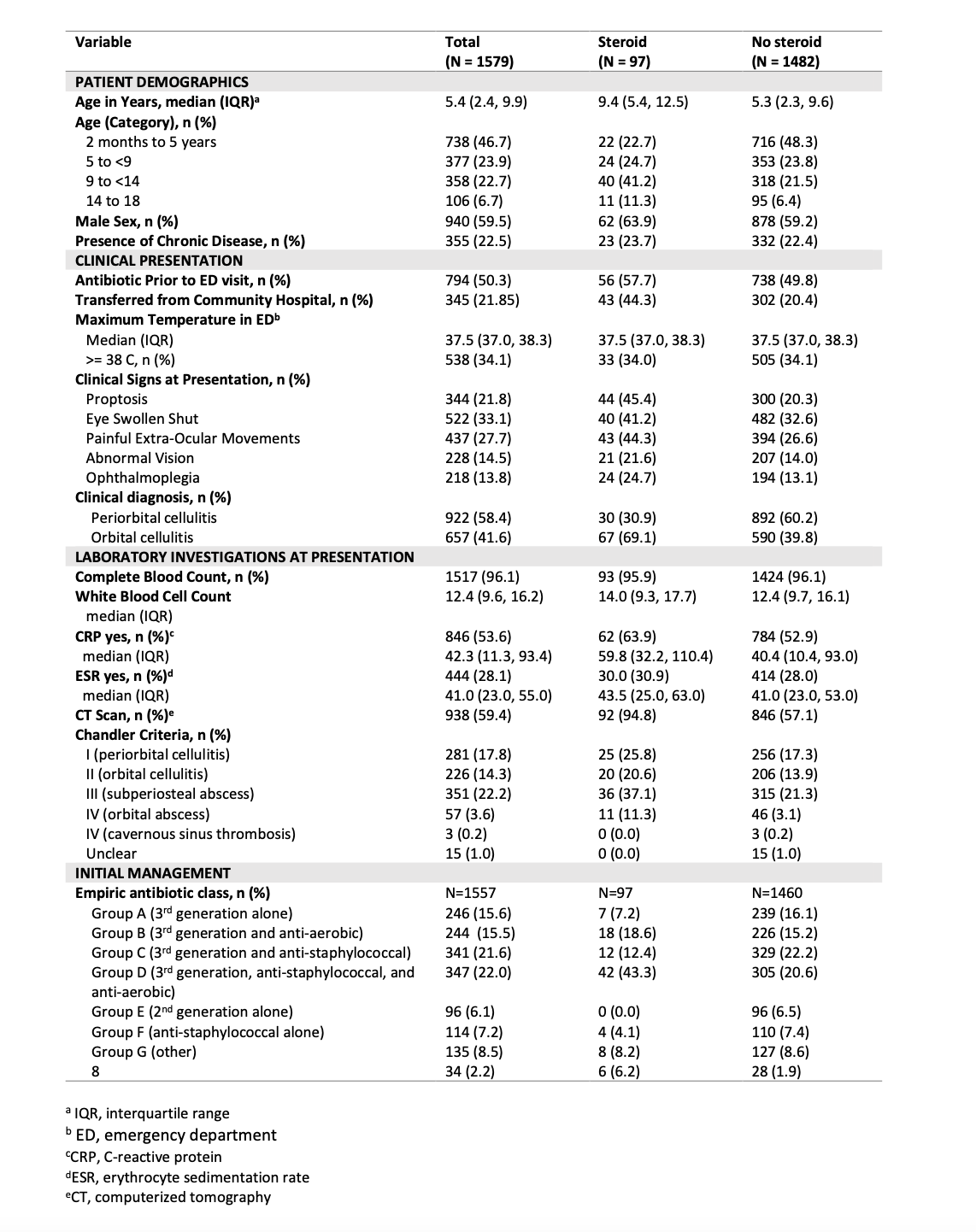
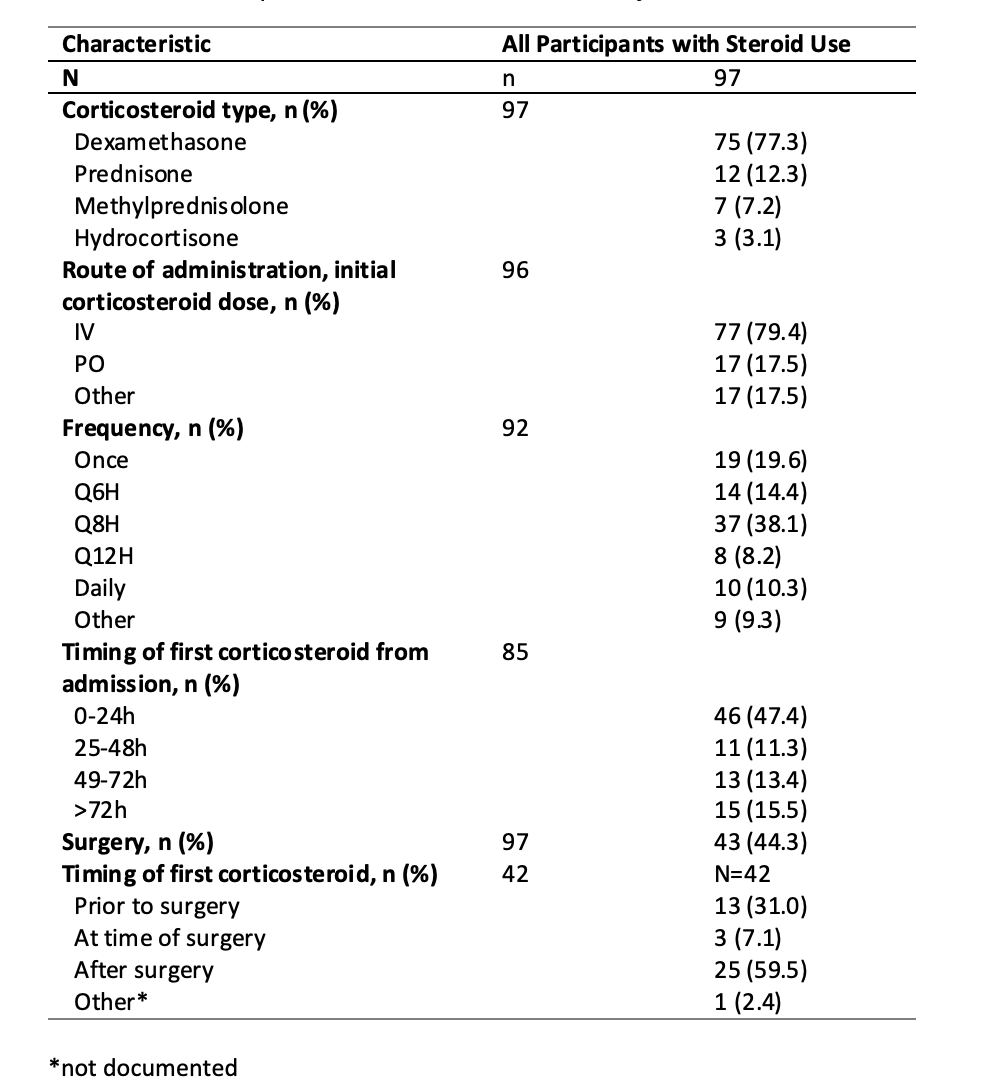
Design/Methods: Multi-site retrospective cohort study of children between 2 months and 18 years of age hospitalized with periorbital and orbital cellulitis across 10 hospitals in Canada between January 1, 2009 and December 21, 2018. Baseline demographics and clinical characteristics were obtained from hospital medical records. The exposure was defined as systemic corticosteroids at any time during the hospital admission, and further classified as either early (≤24 hours after admission) or late (>24 hours after admission). The primary outcome was length of hospital stay and the main secondary outcome was surgical intervention. Other secondary outcomes evaluated included complications, ICU admission, repeat ED visits, and readmission to hospital.
Results: Of the 1579 hospitalized patients, 940 (59.5%) were male and median age was 5.4 years (IQR 2.4-9.9). Median length of stay was 87.2 hours (IQR 54.0-141.3) and 189 (12.0%) underwent surgical intervention. Systemic corticosteroids were used in 97 (6.1%) patients, including in 42/189 (22.2%) who had a surgical procedure. Of the 97 patients, half (n=46, 47.4%) received systemic corticosteroids within the first 24 hours of admission. Of those who also underwent surgery, 3/42 (7.1%) received systemic corticosteroids during surgery and 25/42 (59.5%) received steroids after surgery. Children who received systemic corticosteroids were likely to have clinical signs of orbital cellulitis and be transferred from a community hospital. Median length of stay for children who received systemic corticosteroids was 172.9 hours (IQR 93.5-234.2) versus 83.9 hours (IQR 53.2-134.7) for those who did not receive systemic corticosteroids.
Conclusion(s): In a large cohort of hospitalized children with severe orbital infections, adjunctive systemic corticosteroids were used infrequently, and often during or after surgery. There is limited evidence to support the routine use of systemic corticosteroids.
.png)
