Technology
Session: Technology 1
166 - Feasibility of Postoperative Pediatric Telemedicine in Nunavik: A Mixed Methods Study
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 166
Publication Number: 166.2005
Publication Number: 166.2005

Adalet Bugra (she/her/hers)
Medical student
McGill University Faculty of Medicine and Health Sciences
Saint-Laurent, Quebec, Canada
Presenting Author(s)
Background: Inuit children from Nunavik, to access surgical care, are relocated by plane to the Montreal Children’s Hospital. A follow-up appointment is made a few days post-discharge. As per our hospital-wide audit, 4.1% of pre-operative consults and postoperative follow-ups are done via telemedicine. Because medical relocations can have significant impact on patients and their families, we wanted to explore the technical and operational feasibility of pediatric telemedicine in the postoperative context in Nunavik.
Objective: To determine the feasibility of pediatric postoperative telemedicine follow-ups in Nunavik following surgery at the Montreal Children’s Hospital.
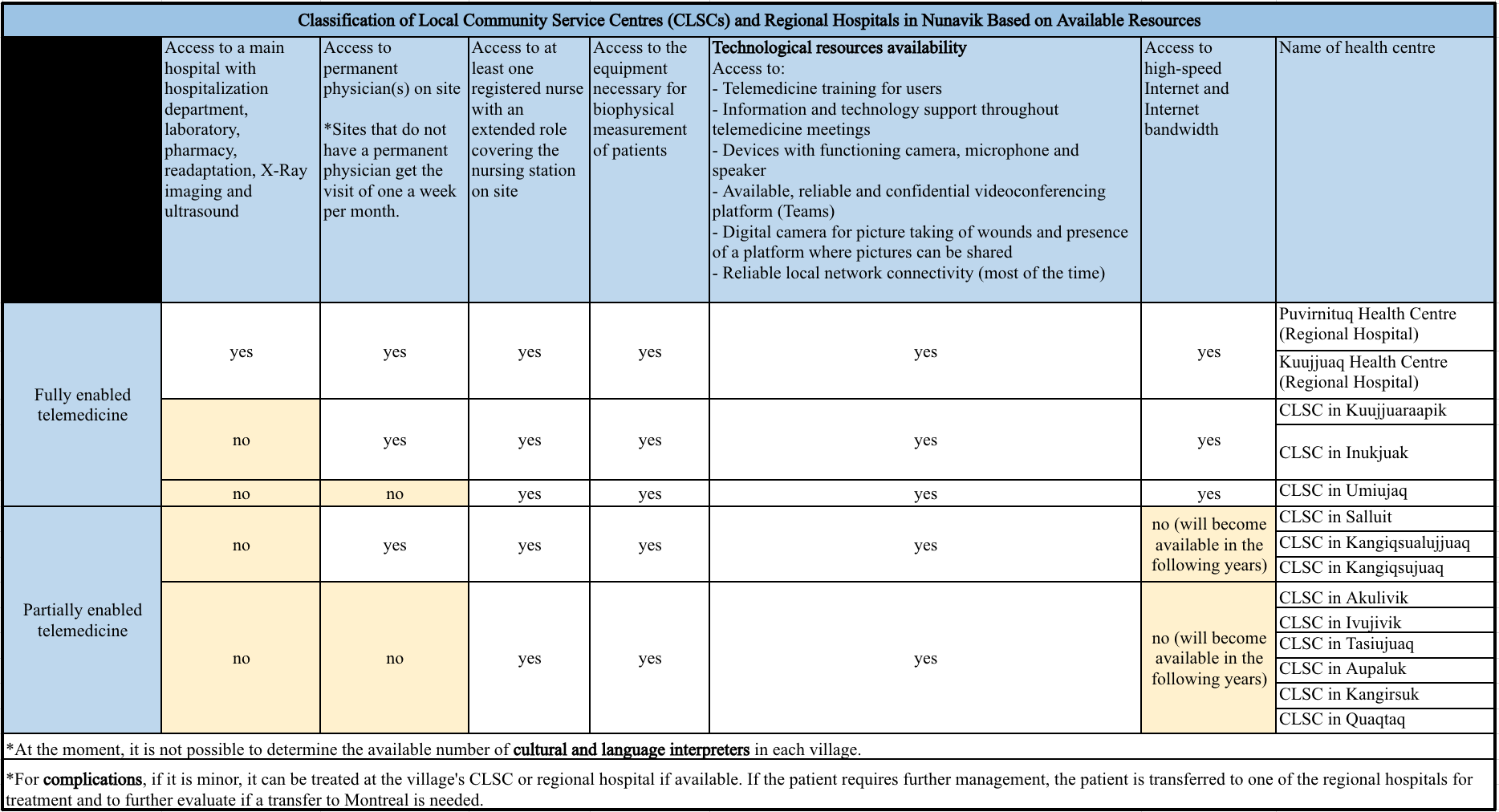
Design/Methods: In this mixed methods study (August 2022 - March 2023), we recruited ten healthcare providers who regularly interact with Inuit families of Nunavik. We conducted individual semi-structured in-depth interviews about postoperative care in this setting and analyzed the data thematically. In parallel, we conducted a narrative synthesis of the literature to assess the potential technical and operational resources needed to enable postoperative telemedicine in the region. We then determined the capability for telemedicine in each of the fourteen villages of Nunavik using data provided by the Nunavik Regional Board of Health and Social Services.
Results: From the interviews, among the main themes influencing the feasibility of telemedicine were 1) general considerations for telemedicine use as a follow-up modality, 2) patient characteristics most suitable for postoperative telemedicine, 3) resources needed for telemedicine use as a follow-up modality, 4) the collaboration between the different stakeholders involved in the care of Inuit children, 5) the feasibility of postoperative telemedicine as determined by healthcare providers. All interviewees deemed pediatric postoperative telemedicine in this region feasible but highlighted conditions for its success. As of January 2023, the two regional hospitals and three health centers of Nunavik had full capabilities for postoperative telemedicine. The nine remaining health centers had partial capabilities mainly due to limited access to stable high-speed Internet and Internet bandwidth.
Conclusion(s): Postoperative pediatric telemedicine is feasible in the remote region. Leveraging centres with appropriate capacity would allow the increase in telemedicine usage in Nunavik. Engaging in discussions with families is primordial to ascertain whether it aligns with their preferences and to respect their autonomy.