Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 5
275 - Social Needs Screening and Referral Practices Across Pediatric Primary Care Practices in Maryland
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 275
Publication Number: 275.1348
Publication Number: 275.1348

Hanae Fujii-Rios, MD MPH (she/her/hers)
Assistant Professor
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: There is ongoing interest and focus on addressing health-related social needs (HRSN), with recent regulatory bodies requiring screening in certain settings. Though not yet included in the new requirements, pediatric primary care has been at the forefront. Assessing statewide practices is important to ensure patients and families receive services to address HRSNs.
Objective: To characterize HRSN screening and referral processes amongst a representative sample of pediatric primary care practices in Maryland.
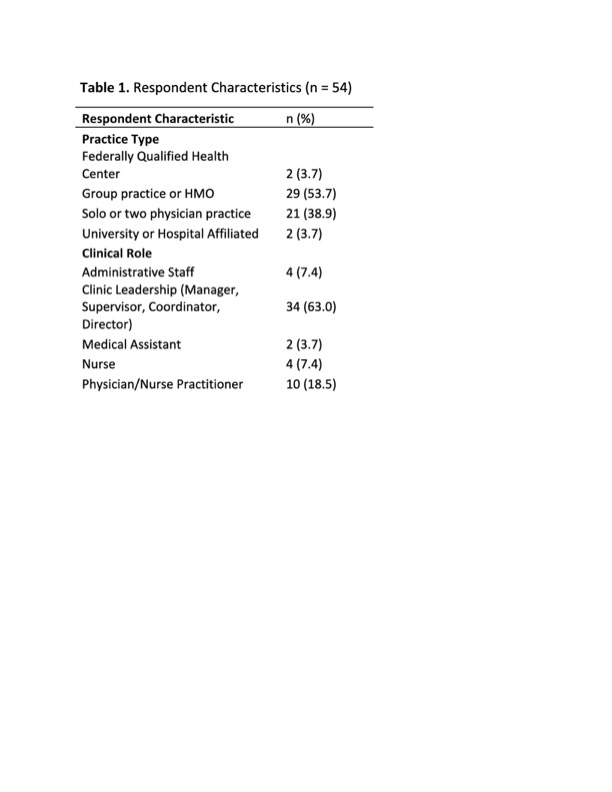
Design/Methods: A survey was developed by content experts and included questions about practice characteristics, HRSN screening content and administration processes, and referral mechanisms. A comprehensive list of practices was developed from Data Axle Reference Solution database, Google Map using a generic webpage crawler, and lists from Maryland Behavioral Health Integration in Pediatric Primary Care, Maryland Health Care Commission and Baltimore City Health Department. From June 1, 2023 to August 31, 2023, two study team members called clinics and requested survey completion by email, over the phone or fax by the individual most knowledgeable about screening practices. Efforts were made to obtain a sample proportional to the pediatric population density within each of the 24 counties in Maryland. Results were summarized using descriptive statistical analysis.
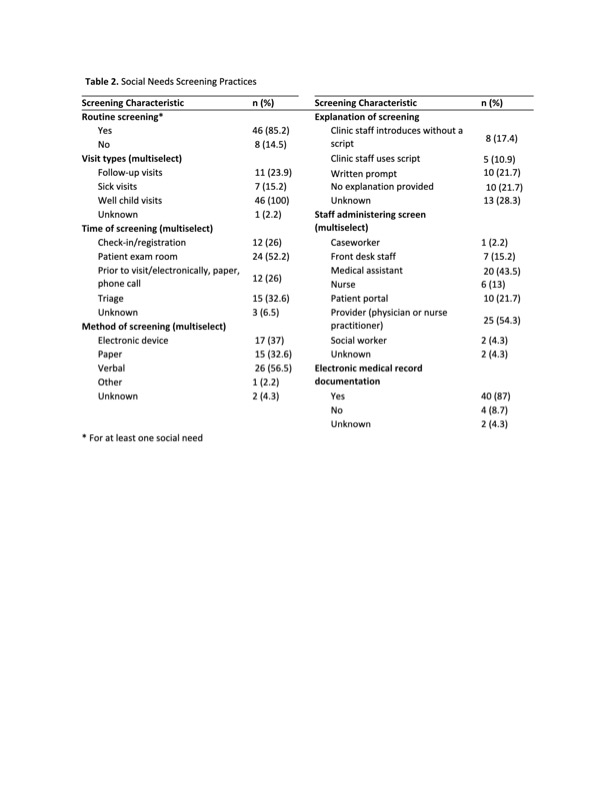
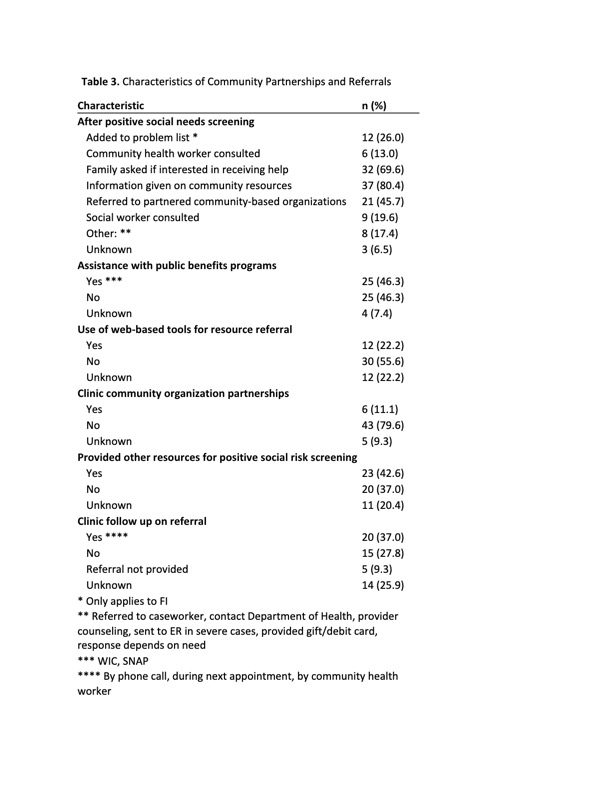
Results: 54 practices from 23 of the 24 Maryland counties completed surveys. Practice types included group vs. solo or two physician practices, federally qualified health centers, and university or hospital affiliated practices. Of the 85% of practices reporting screening for at least one HRSN, all screen during well child visits, 24% during follow-up visits, and 15% during sick visits. Screening is performed at multiple points during visits, with most occurring in the exam room (52%), verbally (57%), and by a physician or nurse practitioner (54%). The most screened HRSNs included personal safety (70%), housing (54%), food (52%), childcare (48%), and education (48%). Most practices document HRSN in the electronic medical record (84%) and 70% ask if caregivers would like resource assistance. Clinics have various cascading interventions including referrals to community resources, social work and community health workers.
Conclusion(s): Most practices universally screen for at least one HRSN though variability exists in how and when screening occurs. Further characterizing the context of screening practices at a statewide level would be beneficial to ensure successful implementation of screening and referral mechanisms.