Hospital Medicine
Session: Hospital Medicine 2
324 - Keiki COVID-19 Chronicles: Characteristics of Pediatric COVID-19 Hospital Admissions in Hawai`i
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 324
Publication Number: 324.365
Publication Number: 324.365

Shelby Tadaki (she/her/hers)
Student Researcher
Hawaii Pacific Health
Honolulu, Hawaii, United States
Presenting Author(s)
Background: Coronavirus disease 2019 (COVID-19) has been studied globally since its identification in December 2019. In Hawai’i, data between March 1, 2020 and February 28, 2021, revealed that the Pacific Islander community, which comprises 5% of the state’s population, disproportionately accounted for 22% of COVID-19 cases and deaths. These statistics were primarily reflective of adult patients as the adult population was affected earlier in the pandemic. However, according to the American Academy of Pediatrics, pediatric cases now account for 17.9% of all cases since the onset of the pandemic. Data specific to the pediatric Hawai’i population has not been studied.
Objective: This study aims to investigate hospitalized pediatric COVID-19 patients in Hawai’i's only tertiary pediatric hospital, focusing on the unique characteristics of this population.
Design/Methods: A retrospective chart review of children ages 0-18 years presenting to Hawai’i Pacific Health facilities with a final diagnosis of COVID-19 between April 2020 and June 2023 was conducted. Descriptive statistics were employed to describe the inpatient pediatric COVID-19 population. Univariate analysis and multivariable logistic regression were used for comparison.
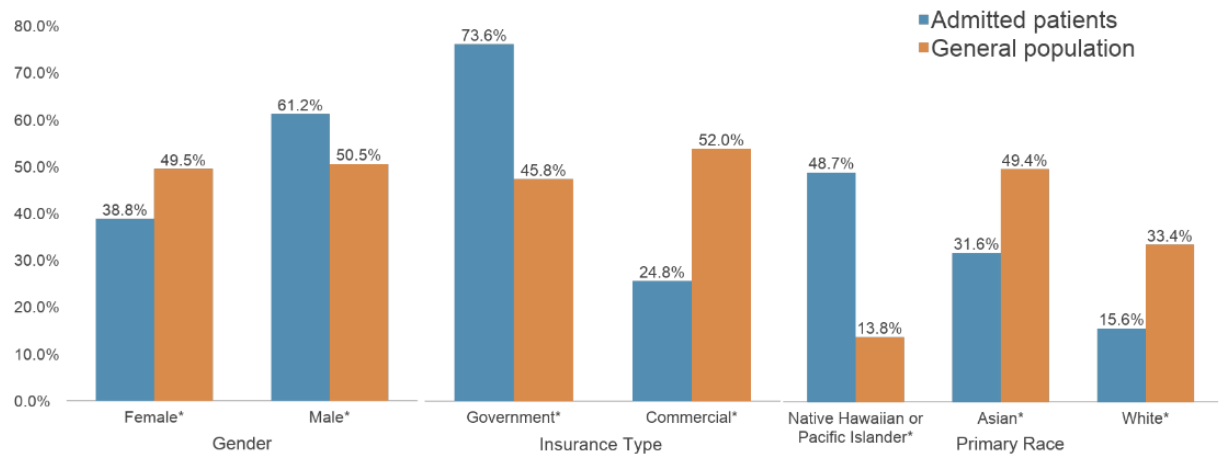
Results: Of the 307 COVID-19 encounters, 61.2% were male (n=188), 48.7% were Native Hawaiian or Pacific Islander (n=150) and the average length of stay was 5.8 days. The primary reasons for hospitalization were respiratory (45.3%), neurologic (14.0%), and gastrointestinal (12.7%). Males (p=0.0002), Native Hawaiians or Pacific Islanders (p < 0.0001) and those with government insurance (p < 0.0001) were more likely to be admitted when compared to Hawai’i’s general pediatric population (see Figure 1). Geographically, higher case concentrations were found in certain zip codes on Oahu: Waianae, Waialua, metropolitan Honolulu, and Kaneohe. Of the pediatric hospitalized cases with COVID-19, 43.3% of patients had 0 comorbidities, 24.8% had 1 comorbidity, and 31.9% had 2 or more comorbidities.
Conclusion(s): This study reveals distinct patterns that could guide targeted interventions for pediatric patients with COVID-19 in Hawai’i. Males, Native Hawaiians or Pacific Islanders, and those with government insurance were more likely to be hospitalized, with particular geographic areas in Hawai’i exhibiting higher concentrations of cases. Understanding the unique characteristics of pediatric COVID-19 patients in Hawai'i can facilitate more precise and timely interventions for those patients at highest risk.