Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 3
11 - Reducing neonatal surgical site infections: a quality improvement project
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 11
Publication Number: 11.3012
Publication Number: 11.3012
Huayan Zhang, MD
Neonatologist
Children's Hospital of Philadelphia/Guangzhou Women and Children's Medical Center
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: As a major cause of health care-associated infections, surgical site infection (SSI) is a costly and challenging complication of postoperative neonates. It is the most common health care-associated infection (HAI) in low and middle-income countries, with an overall incidence of 11.8% (1.2%~23.6%). In high-income countries, the incidence of SSI ranges from 1.2% to 5.2%. And as reported, SSI is associated to the risk of mortality. Despite efforts of sterilization in the operating room, the rate of SSI remains high in our Surgical Neonatal Intensive Care Unit(SNICU)averaging 14.4% from October 2022 to March 2023,worse than the situation in most developing countries. Therefore, we decided to begin a quality improvement (QI) project about SSI in our SNICU.
Objective: This single center QI project identifies and implements specific clinical practices to reduce SSI by 20% over a 6-month period.
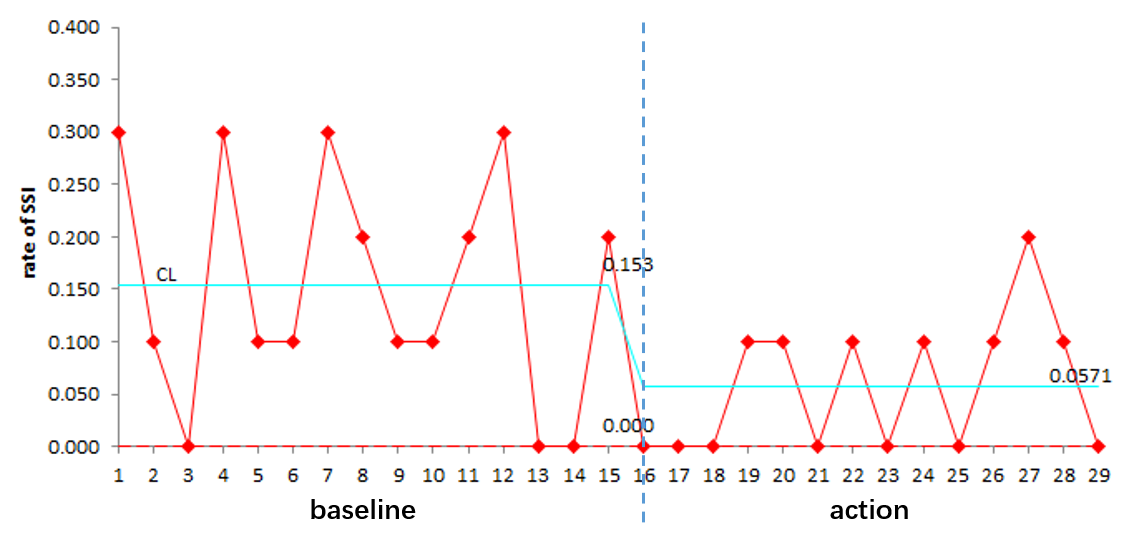
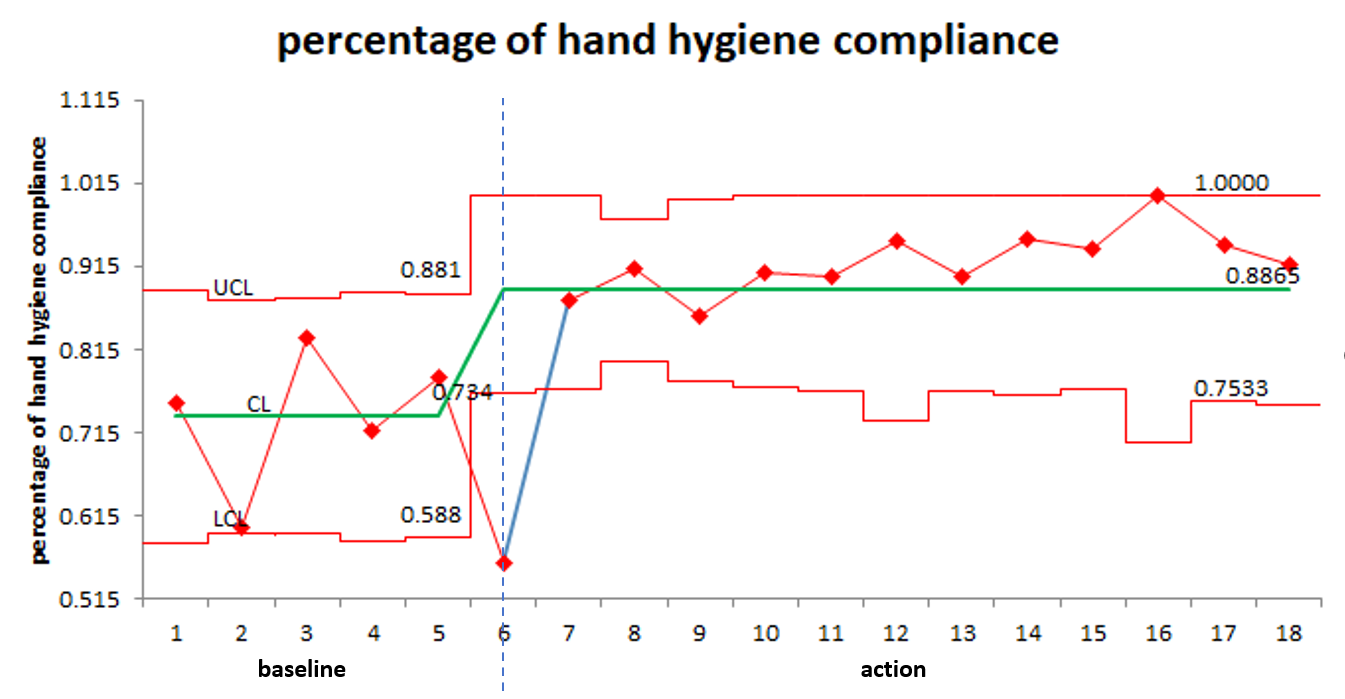
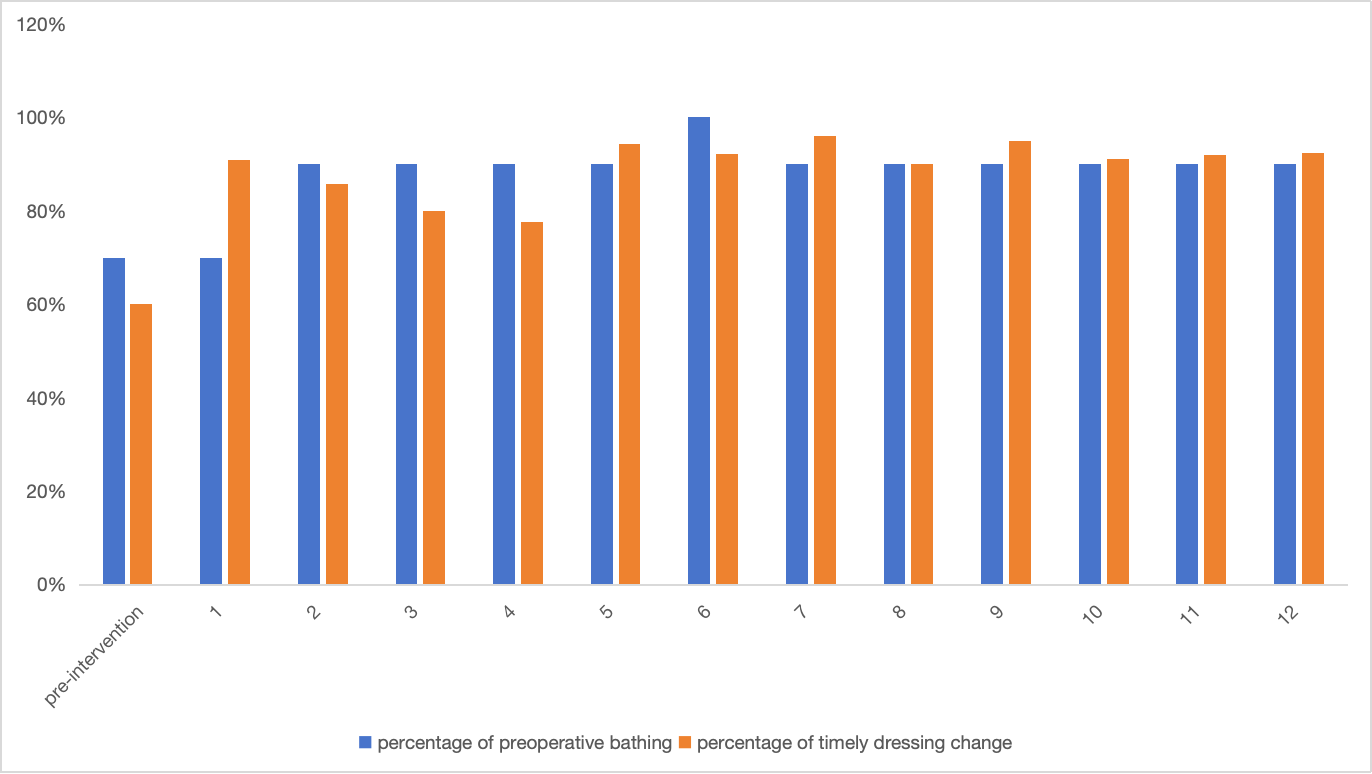
Design/Methods: A multidisciplinary QI team including pediatricians of SNICU/intensive care unit (ICU)/respiratory department/emergency/cardiac intensive care unit, oral surgeon and neonatal nurses was gathered. Through baseline data collection, literature review, and multiple team discussions, members of the multidisciplinary QI team determined the key drivers that influence the rate of SSI, including preoperative bathing, poor hand hygiene and improper wound dressing change. Then a series of interventions were implemented through plan-do-study-act (PDSA) cycles. Main interventions included: improving preoperative bathing, enhancing hand hygiene compliance, and timely and proper surgical wound dressing change. Along with the application of interventions mentioned above, the proportion of SSI per 10 consecutive surgical wounds over a 30-day period was collected to assess the primary outcome. Process measures included hand hygiene compliance and the rates of preoperative bathing and timely dressing change.
Results: During this QI project period, there were 120 surgical sites in total, and the rate of SSI decreased by 57.2%, from a baseline of 14.4% to 6.15% by September 2023. There were significant improvements in hand hygiene compliance, preoperative bathing, and timely dressing change. The percentage of hand hygiene compliance increased from 60% to 100%, the percentage of preoperative bathing rose from 70% to 100%, and the percentage of timely dressing change went up from 60% to 94.4%.
Conclusion(s): It is possible to reduce SSI by certain practices implemented properly. Key practices the effective in our unit include preoperative bathing, improving hand hygiene compliance and timely postoperative dressing change.