Hospital Medicine
Session: Hospital Medicine 2
316 - Characteristics of Patients With Multi-System Inflammatory Syndrome in Children (MIS-C) by Disease Severity: The Experience of a Medium-Sized Children’s Hospital
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 316
Publication Number: 316.376
Publication Number: 316.376

Jordan Kurzum, MD (he/him/his)
Resident
St. Christopher's Hospital for Children
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: In March 2020 the United States recorded its first COVID-19 case, leading to significant changes both for the US healthcare system and society. Just a month later, the first case of MIS-C emerged as a post-infectious systemic inflammatory syndrome with the potential to cause severe morbidity and mortality in children. Initially described as resembling Kawasaki disease in a cohort of eight patients, MIS-C is now defined by the CDC using specific clinical, laboratory and epidemiologic linkage criteria:
1. Clinical criteria: fever > 38.0C, clinical severity leading to hospitalization or death, evidence of systemic inflammation (CRP > 3.0mg/dL), and new onset manifestations in at least two organ systems
2. Laboratory criteria: detection of COVID-19 via PCR or antigen test within 60 days of diagnosis or detection of COVID-19 antibodies
3. Epidemiologic Linkage Criteria: close contact with a known or suspected patient with COVID-19 in the preceding 60 days.
Because of MIS-C’s novelty and rarity, characterizing its severity has relied on expert opinion and preliminary studies. While several studies have used a combination of clinical and laboratory criteria to assess MIS-C severity, conflicting results have contributed to a knowledge gap.
Objective: Evaluation of demographic, clinical, and laboratory factors and their relation to disease severity in patients with MIS-C.
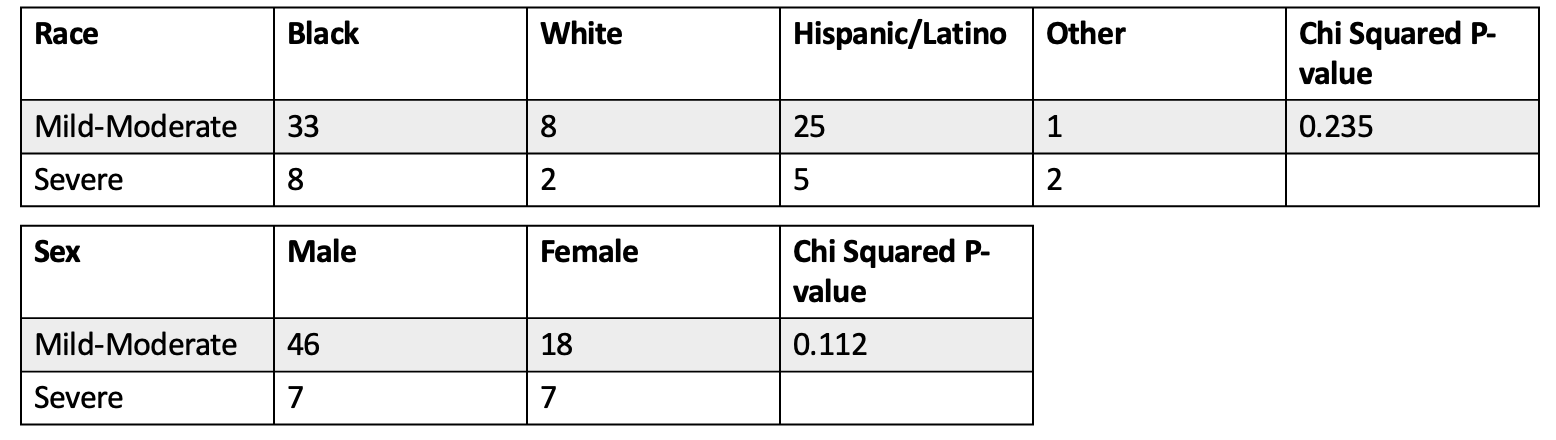
Design/Methods: We conducted a retrospective chart review of MIS-C patients admitted to St. Christopher’s Hospital for Children from April 2020 to April 2022. Analysis was completed with ANOVA and Chi Squared tests using SPSS software. We categorized illness severity as mild to moderate (requiring hospitalization without PICU stay) and severe (requiring PICU stay).
Results: Eighty one patients were included in this study. We found statistically significant associations between severe MIS-C and elevated d-dimer (p < 0.001) and troponin (p < 0.001), decreased platelet count (p = 0.035) and hemoglobin (p = 0.004), and increased BMI (p = 0.009). Patients with severe MIS-C were also more likely to have a prolonged hospital stay (p < 0.001). Other factors, including PT, PTT, fibrinogen, CRP, ferritin, lymphocyte count, BNP, age, and race were not found to have any statistically significant distinction between mild to moderate and severe MIS-C.
Conclusion(s): Our findings reveal several clinical, laboratory, and demographic factors associated with worse MIS-C disease severity. Further studies are required to provide a deeper understanding of the relationships between clinical, laboratory, and demographic characteristics and MIS-C disease severity.
.png)