Child Abuse & Neglect
Session: Child Abuse & Neglect 1
181 - Trends in Service Utilization Among Youth Within the Child Welfare System
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 181
Publication Number: 181.1336
Publication Number: 181.1336
- FB
Farah W. Brink, MD (she/her/hers)
Assistant Professor
Nationwide Children's Hospital
6741 Baronet Blvd Dublin OH 43017, Ohio, United States
Presenting Author(s)
Background: An estimated 600,000 children were victims of abuse and neglect in 2021. A recent study found that a history of child maltreatment was associated with an increased likelihood of hospital admission with mental health (MH) care needs and required more consultations with specialized healthcare professionals. Disruptions in the home may lead to disruptions in healthcare insurance coverage and thus access to routine care and more specialized services. Current literature on the types of healthcare that youth within the child welfare system are accessing is split, though their presentation to emergency departments (EDs) remains higher than their peers without maltreatment.
Objective: To examine the trends in service utilization among children living in Ohio within the child welfare system.
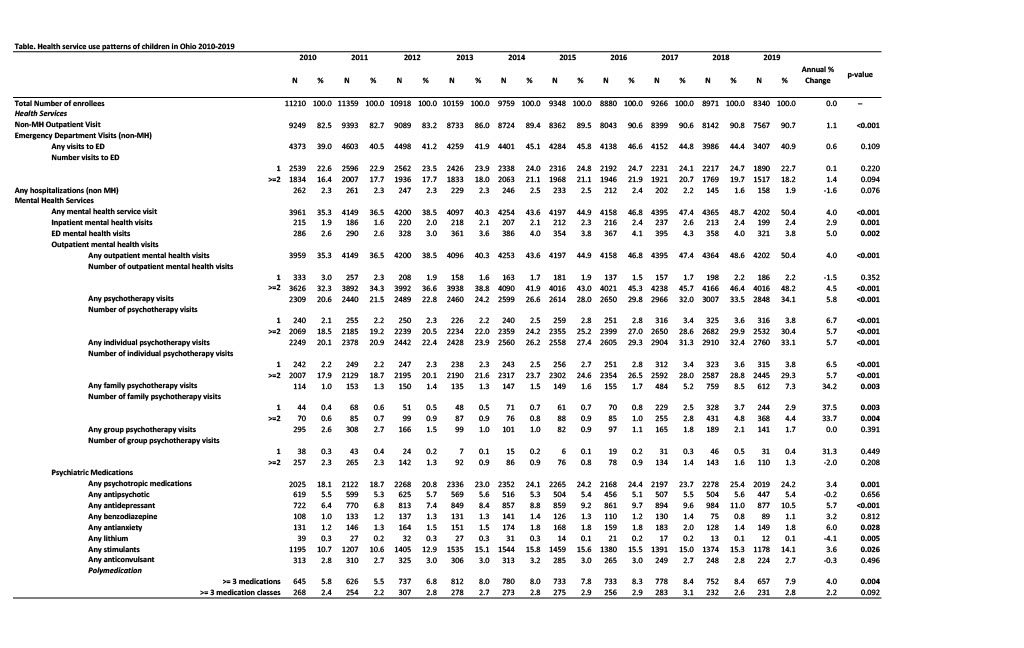
Design/Methods: This retrospective cross-sectional study included youth 5-17 years who had their first child welfare case opened between 2010-2019 in Ohio. The Statewide Automated Child Welfare Information System provided data regarding open child welfare cases and Ohio Medicaid claims provided service utilization data including number and types of psychiatric diagnoses, MH visits, ED visits, hospitalizations, and use of psychotropic medications. Cases were identified at the time of their open case and service use over the following one year was abstracted. Logistic regressions were performed to test trends over time in demographic and clinical characteristics and service utilization.
Results: Between 2010-2019, there was an average of 9821 enrollees per year. The number of MH diagnoses increased from 38.1% to 53.7%. We found significant increases in common disorders including ADHD, autism, adjustment disorders, communication and learning disorders, depression, intellectual disability, and specifically anxiety diagnoses which surged from 4.0% to 13.6%. Overall, youth receiving MH services rose from 35.3% to 50.4%, with steady increases in outpatient, inpatient, and ED visits. Overall, psychiatric medication utilization increased as well, especially in antianxiety (6.0% average annual increase), antidepressants (5.7%), and stimulants (3.6%), while lithium’s usage decreased by 4.1% annually [Table].
Conclusion(s): Health service utilization increased significantly for this population overall but rose especially for all MH services including ED visits. This confirms greater MH services need provided for children in the child welfare system receiving Medicaid. State and national policies supporting the MH service reimbursement and expansion of the provider network should be considered to address this growing need.