Cardiology
Session: Cardiology 1
145 - Pulse Oximetry Screening for Critical Congenital Heart Disease at a Referral Hospital in Jordan
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 145
Publication Number: 145.3001
Publication Number: 145.3001

Naser Aldain Abu Lehyah, MD (he/him/his)
Pediatric Specialist-NICU division
Division of Neonatology, Department of Pediatrics, Maternity and Children’s Hospital at Al Bashir Hospitals, Amman, Jordan
Presenting Author(s)
Background: Early studies, largely from Europe, provided the initial evidence for the efficacy of screening for critical congenital heart disease (CCHD) with pulse oximetry. Meta-analyses have since found specificity for CCHD of 99.9%, sensitivity of about 76%, and a false positive rate of 0.14%. It is now mandated in all states in the US and many high-income countries. However, challenges in implementation in low- and middle-income countries (LMICs) have been encountered, meaning many children are identified later by astute clinicians or when symptoms develop. This may lead to later diagnosis and worse outcomes.
Objective: To pilot screening for CCHD with pulse oximetry at a tertiary hospital in Jordan. We aimed to both identify barriers to implementation for a larger project as well as characterize cardiac disease identified by screening.
Design/Methods: Consecutive newborns born at Al Bashir Hospital in Amman, Jordan were screened with pulse oximetry according to the current American Academy of Pediatrics screening algorithm. Infants who failed pulse oximetry screening underwent an echocardiogram by a pediatric cardiologist. Demographic and clinical data were recorded at the time of screening.
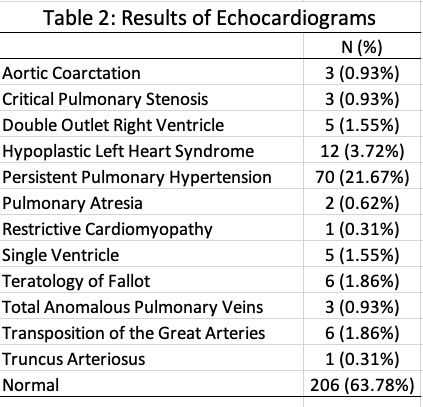
Results: A total of 7,795 newborns were screened from January 1, 2023, to October 15, 2023 (Table 1). The majority were screened at or after 24 hours of age (N=4520, 58.0%). A total of 323 (4.14%) failed pulse oximetry screening and ultimately had an echocardiogram performed. Among 323 echocardiograms performed, abnormalities were found in 117 children (36.2%; Table 2). This included 46 cases of CCHD, yielding a rate of 5.9 per 1,000 live births. Only 21 patients with CCHD (45.7%) had a prenatal diagnosis. In addition to CCHD, screening identified 38 infants with pneumonia, 56 with sepsis, and 70 with persistent pulmonary hypertension (PPHN). The false positive rate for CCHD was 3.55%, and the false positive rate for any clinically important finding was just 1.44%. Only six families (0.08%) refused screening.
Conclusion(s): Pulse oximetry screening for CCHD was successfully implemented in a referral hospital in Jordan. This identified 25 patients with previously unknown CCHD who may have otherwise been discharged. The rate of CCHD was substantially higher than international averages. Screening also identified a high number of other conditions requiring intervention or extended monitoring. Screening was acceptable to families with very few refusing screening.
.jpg)