Infectious Diseases
Session: Infectious Diseases 1
575 - Ethnic and Racial Differences in Children with Respiratory and Neurological Post-Acute Sequelae of SARS-CoV-2
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 575
Publication Number: 575.388
Publication Number: 575.388

Suchitra Rao, MBBS, MSCS (she/her/hers)
Associate Professor
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Minority children are at greater risk for acute COVID infection, but it is uncertain whether this increased risk exists for certain post-acute sequelae of SARS-CoV-2 (PASC) in children.
Objective: To compare the risk of neurologic and respiratory manifestations of PASC in children by sociodemographic and clinical characteristics including social drivers of health (SDOH).
Design/Methods: We conducted a retrospective cohort study of patients < 21 years seeking care at one of 41 PCORnet health systems across the US using EHR data from outpatient, inpatient and emergency department settings. We included children with a positive SARS-CoV-2 test (PCR and antigen), or SARS-CoV-2, MIS-C or PASC diagnosis from February 29, 2020-August 1, 2022 and identified children with >/=2 codes associated with respiratory and neurologic presentations of PASC. Associations between sociodemographic and clinical characteristics and respiratory and neurologic outcomes were measured by odds ratios and 95% confidence intervals using multivariable logistic regression models adjusted for age, site, race, ethnicity, area deprivation index, time period of cohort entry, presence and complexity of chronic respiratory or neurologic condition and healthcare utilization.
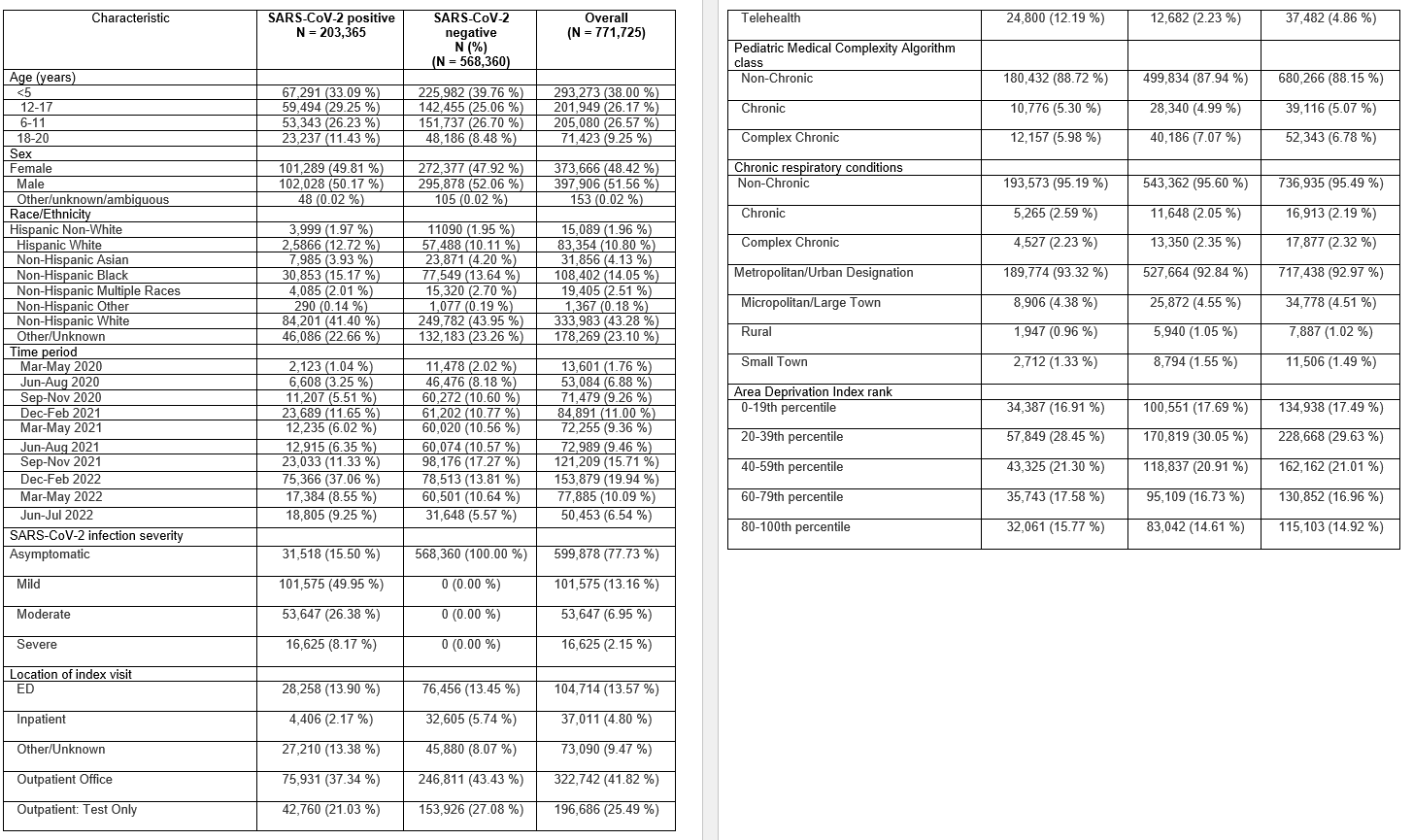
Results: Among 771,725 children in the cohort, 203,365 (26.3%) had SARS-CoV-2 infection. Sociodemographic and clinical characteristics of the cohort are shown in Table 1. Patients with acute SARS-CoV-2 were older, of Hispanic White ethnicity and Black race. Among infected children, 3217 children had respiratory PASC and 2009 children had neurologic PASC. In logistic regression models, children < 5 years (OR 1.80, 95% CI 1.63-1.98), and Hispanic White children (OR 1.20, 95% CI 1.06-1.34) had higher odds of having respiratory PASC. Children living in regions with higher area deprivation indices (OR 1.25, 95% CI 1.10-1.42) for 60-79th percentile and with chronic complex respiratory conditions (OR 3.30, 95% CI 2.92-3.72) had higher odds of respiratory PASC (Figure 1). In contrast, older (OR 1.38, 95% CI 1.17-1.62), non-Hispanic White children and those with underlying complex neurologic conditions (OR 2.05, 95% CI 1.78-2.36) were more likely to have neurologic PASC (Figure 2).
Conclusion(s): Children with underlying respiratory/neurologic conditions were more likely to have these PASC symptoms. Hispanic children and those with higher social deprivation indices were more likely to have pulmonary PASC; these associations were not seen in neurologic PASC. SDOH and related underlying respiratory conditions may disproportionately affect Hispanic children’s risk of respiratory PASC.
.png)
.png)
