Hospital Medicine
Session: Hospital Medicine 2
318 - Comparison of medical hospitalization for suicide attempt or ideation in young adults admitted to a pediatric versus adult hospital
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 318
Publication Number: 318.389
Publication Number: 318.389

Emily L. Jacobson, MD (she/her/hers)
Clinical Assistant Professor
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: The national mental health crisis has led to increased medical admissions for psychiatric conditions in adolescents and young adults. Given their age, young adults can receive care in either pediatric or adult hospitals. Prior studies have found variation in hospital care for a variety of medical conditions based on admitting location, but it is unknown if outcomes differ for those admitted with primary psychiatric disorders.
Objective: To evaluate the effect of hospital type (pediatric versus adult) on the medical care and outcomes for young adults hospitalized with suicidal ideation (SI) or attempt (SA).
Design/Methods: Patients aged 18-25 years old admitted within a single hospital system from 9/1/2017-6/30/2023 for SI, SA, or self-inflicted harm (based on ICD-9 and ICD-10 codes) were identified using an electronic data tool. Patients were excluded if directly admitted to the psychiatric unit; if multiple admissions during the study period, only the first admission was included. Outcomes included admission location, psychiatry and psychology consultation, hospital length of stay (LOS), need for ICU care, discharge disposition, and post-discharge emergency department (ED) visits and hospitalizations. Data were compared via univariate analysis.
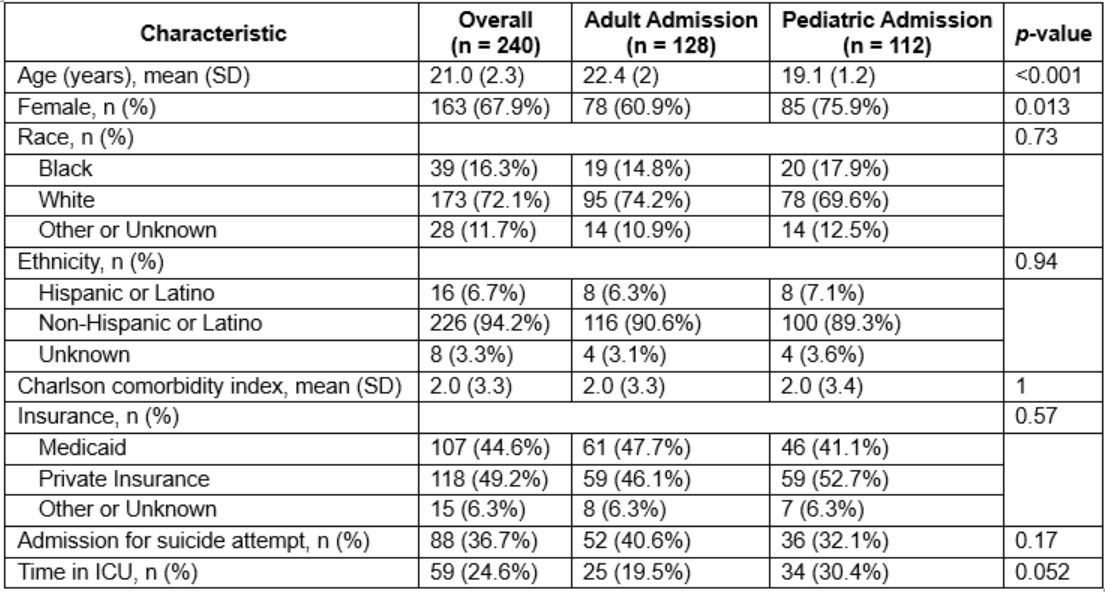
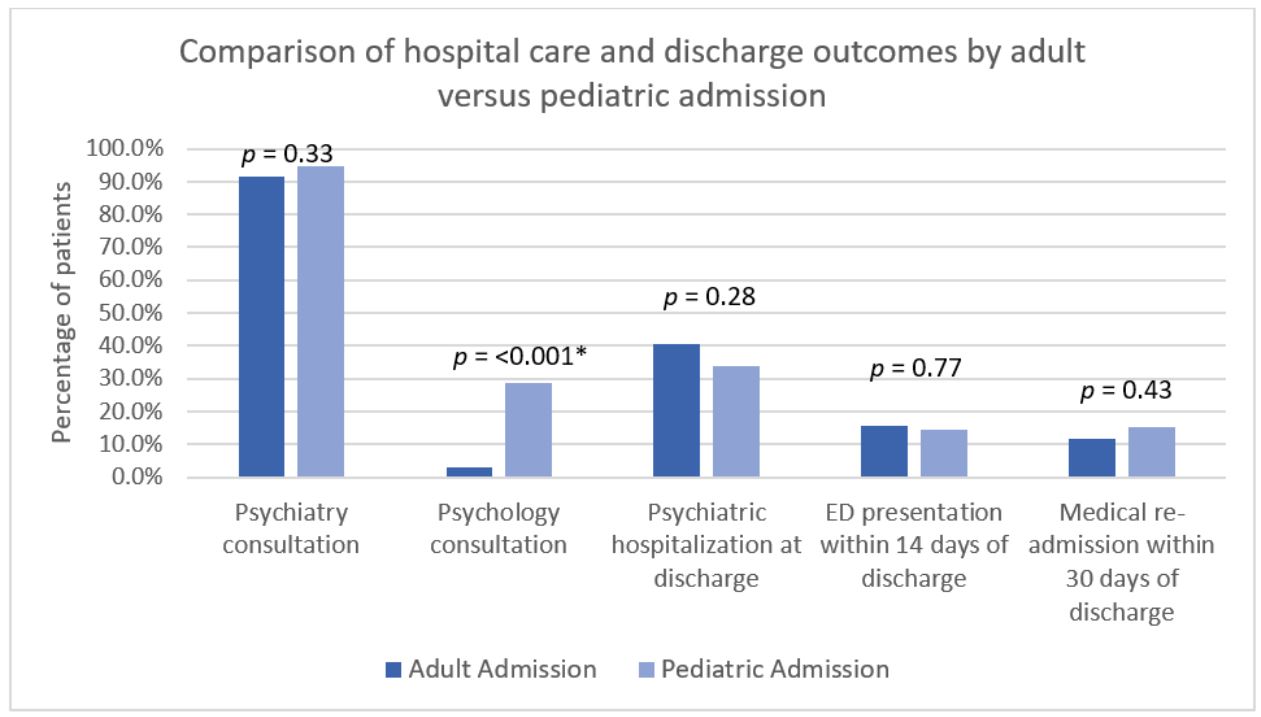
Results: Of the 240 included patient encounters, there were similar rates of admissions to the adult and pediatric hospital (53 vs 47%). Patients admitted to the adult hospital were older (22.4 vs 19.1 years old, p< 0.0001) and less likely to be female (60.9% vs 75.9%, p = 0.013) without a difference in underlying comorbidities (Table 1). While patients admitted to the adult hospital had longer average ED stays prior to medical admission (18.9 vs 9.6 hours, p = 0.005) there was no difference in average hospital LOS (198 vs 184.7 hours, p = 0.69). Nearly all patients had psychiatry consultation (92.9%) but patients admitted to pediatrics had higher rates of psychology consultation (28.6% vs 3.1%, p < 0.0001). There was no difference in discharge location, ED re-presentation, or readmission (Figure 1).
Conclusion(s): Young adults hospitalized for SI or SA were more likely to have longer ED stays and fewer psychology consultations if admitted to an adult versus pediatric hospital. There were no observed differences in other measured short-term hospitalization outcomes. Further work is needed to determine how these differences in care affect hospital throughput, cost, access to care, and long-term outcomes for this population.