Emergency Medicine
Session: Emergency Medicine 10: Trauma
402 - Pain Management of Fractures in the Pediatric Emergency Department: Evaluating for Inequities based on Race, Ethnicity, and Preferred Language
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 402
Publication Number: 402.2990
Publication Number: 402.2990

Christina R. Rojas, MD
Pediatric Emergency Medicine Fellow
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Long bone fractures are a common painful injury for which children seek emergency department (ED) care. Prior studies have demonstrated inequities in pain management for this condition associated with race and ethnicity but have not focused on the association of language preference or timeliness of pain management.
Objective: Evaluate timeliness of pain management by race, ethnicity, and language for children presenting with long bone fractures to the pediatric ED.
Design/Methods: We conducted a retrospective cross-sectional study of ED visits by patients ≤21 years with an ICD-10 code for long-bone fracture, presenting from 2019-2022 to two affiliated pediatric EDs of a tertiary care pediatric hospital. Analyses used Cox regression and restricted mean survival time modeling that adjusted for age, sex, insurance, triage level, mode of arrival, and pain score.
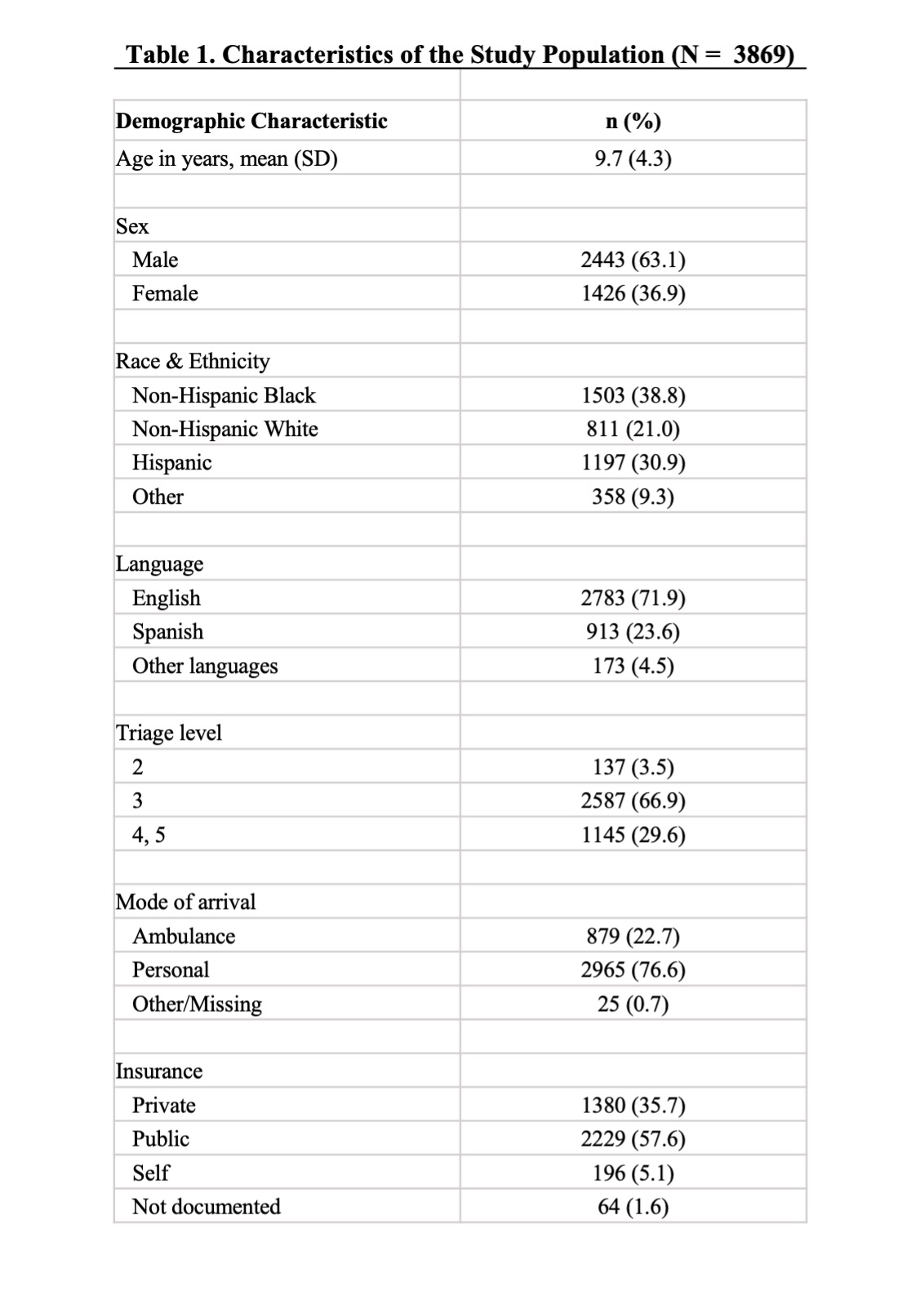
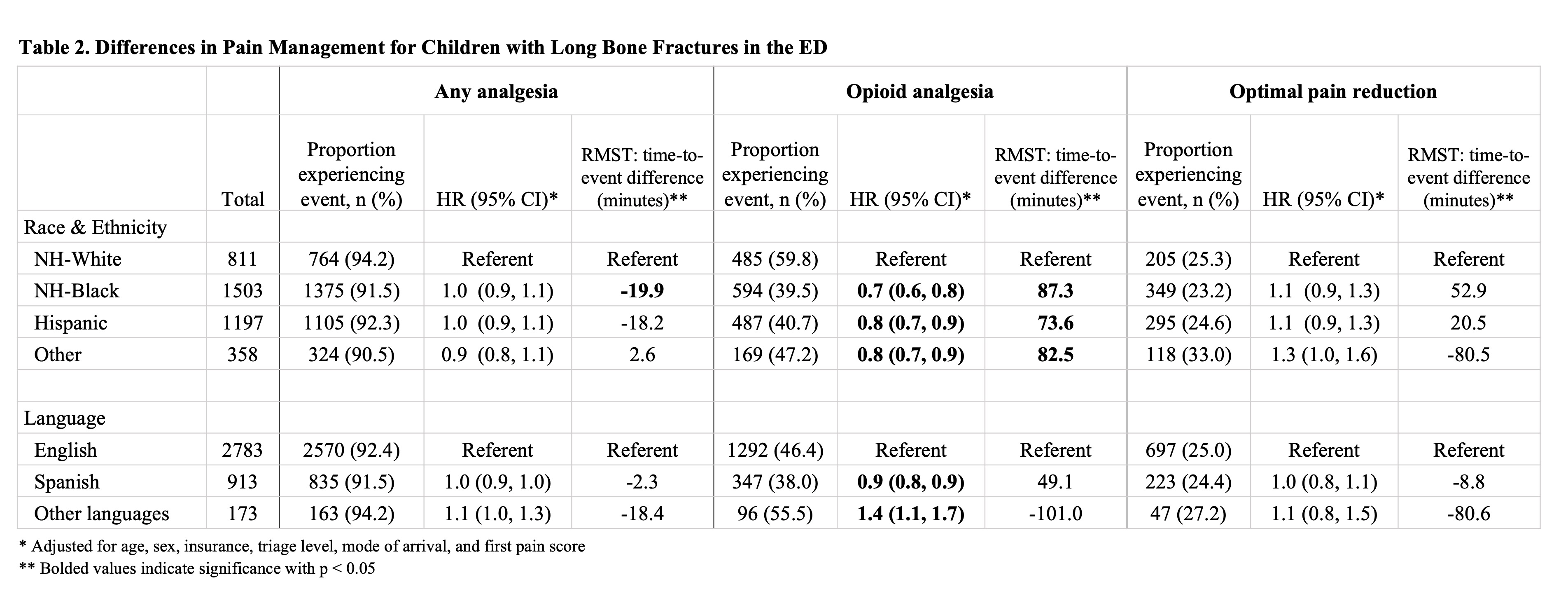
Results: Of 3,869 eligible visits, 38.8% identified as Non-Hispanic (NH) Black, 30.9% Hispanic, 21.0% NH-White, and 9.3% as other races. With regard to language, 71.9% preferred English, 23.6% Spanish, and 4.5% other languages (Table 1). Among these patients, 92.2% received some type of analgesia, 44.8% received opioids, and 25.0% experienced optimal pain reduction, defined as reduction to mild or no pain. Children identifying as NH-Black, Hispanic, and other races were less likely to receive opioid analgesia compared to their NH-White counterparts (hazard ratio [HR] 0.7 [95% CI 0.6, 0.8)]; HR 0.8 [95% CI 0.7, 0.9]; HR 0.8 [95% CI 0.7, 0.9], respectively). These children also waited significantly longer to receive opioid analgesia compared to NH-White children (87.3 additional minutes, 73.6 additional minutes, and 82.5 additional minutes, respectively, all p < 0.05). Children preferring Spanish were less likely to receive opioid analgesia (HR 0.9 [95% CI 0.8, 0.9]), while children preferring other languages were more likely to receive opioid analgesia (HR 1.4 [95% CI 1.1, 1.7]), without significant differences in timeliness. There were no significant differences in optimal pain reduction by race/ethnicity or language (Table 2).
Conclusion(s): There are inequities by race, ethnicity, and language in pain management for children with long bone fractures in the ED, particularly in relation to opioid analgesia and timeliness of pain management. Future efforts should focus on identifying underlying causes for these inequities and developing clinical improvement strategies.