Neonatology
Session: Neonatal Infectious Diseases/Immunology 1
600 - The predictive value of maternal infection biomarkers during the peripartum period for risk assessment of neonatal early-onset sepsis
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 600
Publication Number: 600.405
Publication Number: 600.405
Hugh Simon Lam, MD, FRCPCH
Professor
The Chinese University of Hong Kong
Sha Tin, Hong Kong
Presenting Author(s)
Background: Early-onset sepsis (EOS) remains an important cause of neonatal morbidity and mortality. Maternal inflammation biomarkers may contribute valuable information about neonatal EOS risk, but big data studies related to this has been sparse.
Objective: To assess maternal white blood cell count (WCC), absolute neutrophil count (ANC), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and C-reactive protein (CRP) as predictors of culture-proven neonatal EOS.
Design/Methods: In this multicenter retrospective study in Hong Kong, we included 380,455 mother-infant pairs in Hong Kong (2006-2017). The infants were then tracked for the development of EOS. Maternal CBC and CRP within 48 hours before to 72 hours after delivery were examined in mothers of infants with (n=460) and without (n=379,995) EOS.
Results:
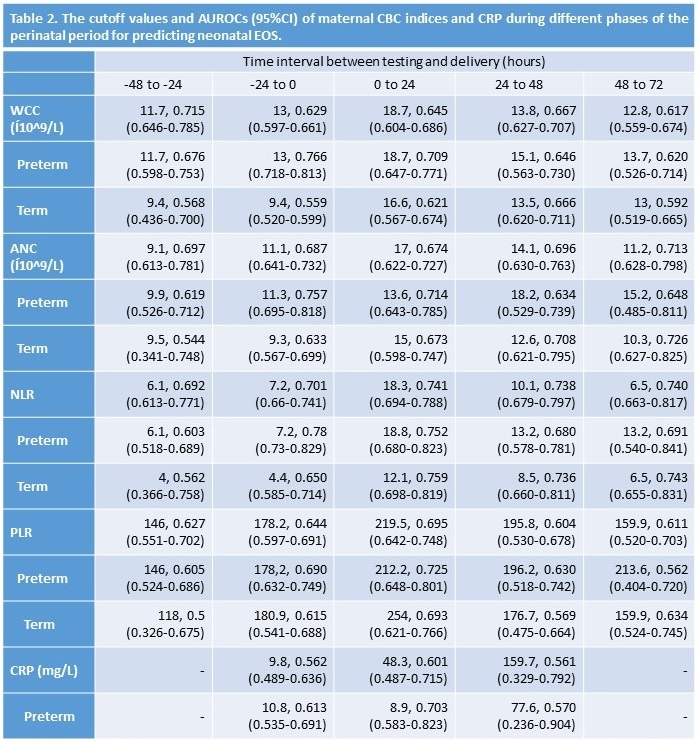
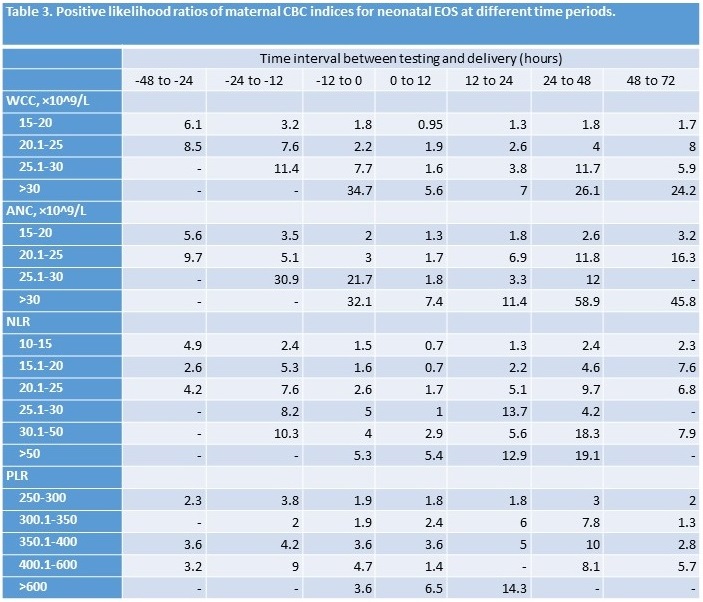
Results: The characteristics of babies born without and with EOS are shown in Table 1. WCC, ANC, NLR and PLR were higher among mothers of infants with EOS (p < 0.001). NLR had the best discriminatory ability for EOS, with area under the receiver operating characteristics curve (AUROC) 0.759 for term deliveries (Table 2). However, standalone diagnostic performance was insufficient for clinical application. Very high maternal WCC (>30×109/L) or ANC (>25×109/L) before delivery had higher likelihood ratios (34.7 and 21.7, respectively) (Table 3).
Conclusion(s): These findings suggest that although maternal biomarkers do not demonstrate sufficient diagnostic performance to be utilized independently, they could enhance multivariate risk assessment tools such as the EOS calculator, which currently does not incorporate maternal biomarkers. Further research should explore the integration of maternal peripartum inflammation markers into EOS risk assessment algorithms to enhance their precision and utility in clinical practice.
.jpg)