Neonatology
Session: Neonatal Infectious Diseases/Immunology 2
609 - Piperacillin-tazobactam versus ampicillin/gentamicin for intraamniotic infection: A propensity-matched non-inferior analysis
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 609
Publication Number: 609.410
Publication Number: 609.410

Katie M. Anderson, MD (she/her/hers)
Resident Physician
The Warren Alpert Medical School of Brown University
Providence, Rhode Island, United States
Presenting Author(s)
Background: In addition to maternal complications, intraamniotic infection (IAI) is associated with acute neonatal morbidity, including early-onset sepsis. Maternal intrapartum antibiotic therapy has a protective effect against the development of neonatal sepsis. However, there is insufficient evidence to support a specific antibiotic regimen to treat IAI.
Objective: To assess whether piperacillin-tazobactam (P-T) is non-inferior to ampicillin/gentamicin (A-G) for the treatment of suspected IAI.
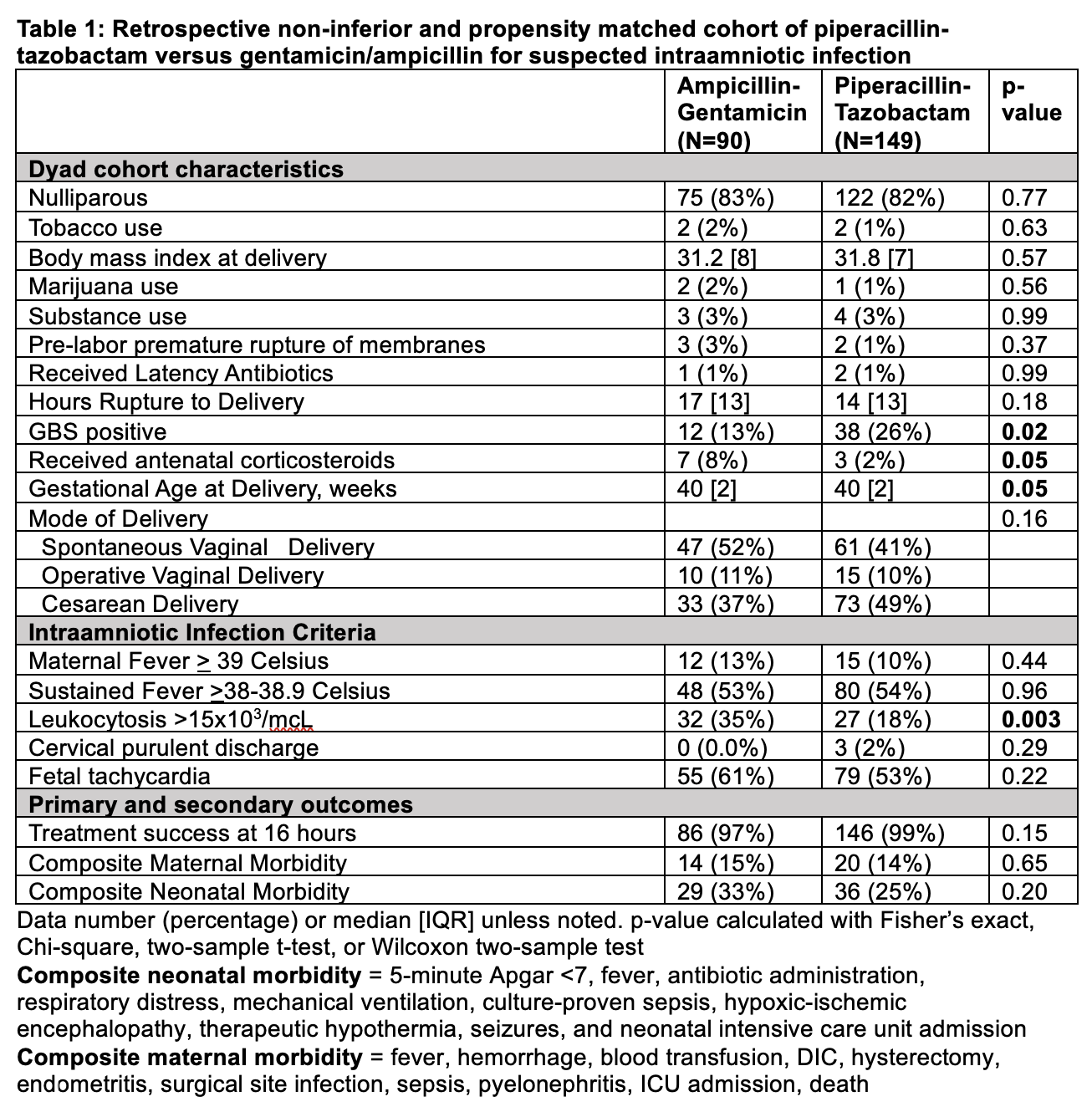
Design/Methods: This was a retrospective cohort study of singleton maternal-neonatal dyads at a single hospital from 12/1/2021– 9/13/2022. Individuals were included if they received either P-T or A-G for suspected IAI, as defined by the American College of Obstetricians and Gynecologists. The primary outcome was maternal treatment success, defined as the resolution of fever within 16 hours of antibiotic administration and the absence of endometritis through 6 weeks post-delivery. With an assumed success rate of 90% for A-G, 126 dyads (63 in each group) were required to conclude with 95% confidence that P-T is, at worst, 15% inferior to A-G. Secondary outcomes were composite maternal and neonatal morbidity. In addition, 1:1 propensity score matching was performed for a subset of dyads based on clinical factors for maternal treatment success (e.g. Group B Streptococcus) using conditional logistic regression to estimate odds ratios (OR) and 95% confidence intervals.
Results: 239 dyads were included: 149 received P-T and 90 received A-G. Generally, the two groups were similar in baseline characteristics. Individuals who received P-T were more likely to be Group B Streptococcus positive and less likely to have received antenatal steroids (Table 1). Treatment success was high in both regimens at 99.32% with P-T and 96.63% with A-G. P-T was 2.69% [-1.07%, 8.77%] more effective at achieving treatment success compared to A-G, and was within the pre-determined non-inferiority limit. Propensity score matching was completed for 80 dyads and there were no significant differences in the treatment success (aOR 2.05 [0.18, 23.10]), composite maternal morbidity (aOR 1.08 [0.46, 2.55]), or neonatal morbidity (aOR 0.64 [0.31, 1.29]).
Conclusion(s): P-T was non-inferior to A-G in achieving maternal treatment success for suspected IAI with similar composite maternal and neonatal morbidity. Further research is needed to assess for effects on long-term complications related to IAI, as well as the impact of specific antibiotic regimens on the neonatal microbiome.