Infectious Diseases
Session: Infectious Diseases 2
65 - Evaluation of an intervention to decrease length of stay in children with low-risk febrile neutropenia
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 65
Publication Number: 65.1310
Publication Number: 65.1310

Molly Rogers, BS (she/her/hers)
Medical Student
St. Jude Children's Research Hospital
Memphis, Tennessee, United States
Presenting Author(s)
Background: Febrile neutropenia is one of the most common serious complications of myelosuppressive chemotherapy. For this reason, pediatric oncology patients with FN have traditionally been admitted to the hospital and started on empiric intravenous antibiotics. However, not all FN patients are at high risk of developing subsequent complications, and a low-risk group exists that could safely be discharged early.
Objective: The objective of this study was to understand if the implementation of new guidelines for treatment of children with low-risk febrile neutropenia at a quaternary pediatric cancer center in the USA decreased the length of hospital stay.
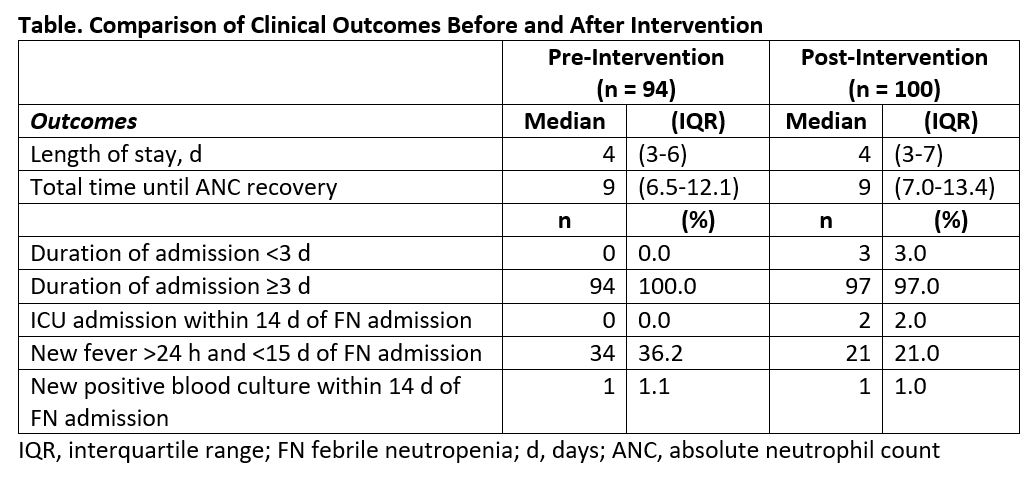
Design/Methods: A retrospective study of 194 FN episodes presenting in pediatric oncology patients at a quaternary pediatric cancer center in the USA. Outcomes of FN episodes were studied and compared before and after early discharge guidelines for low-risk febrile neutropenia (LRFN) were implemented on May 6, 2020.
Results: Total length of hospital stay was similar in the pre- and post-intervention groups (median 4 [IQR 3,6] vs. 4 [IQR 3,7] days, P = 0.443). Differences in adverse outcomes were insignificant between the pre- and post-intervention cohorts, with only two ICU admissions after the first 24 hours inpatient in the post-intervention group, one new positive blood culture (> 24 hours – 14 days of admission) in each group, and 36.2% versus 21% new fever after resolution of initial fever in pre- and post-intervention cohorts respectively. Cumulative antibiotic use between the pre- and post-intervention groups was statistically insignificant (median 13.5 [IQR 22.8,8] vs. 14 [IQR 22,9] days, P = 0.537), whereas Levofloxacin use was significantly longer in the post-intervention cohort versus the pre-intervention cohort (median 0 [IQR 0,4] vs. 0 [IQR 0,0] days, P = < 0.001).
Conclusion(s): The implementation of guidelines for early discharge of LRFN patients showed no reduction in hospital stay. Understanding the optimal strategy for effectiveness of guideline implementation is crucial to improve quality and efficiency of care.