Neonatology
Session: Neonatal Follow-up 3
534 - Health Care Usage Through 2 Years Postnatal Among Extremely Preterm Infants Following Initial NICU Discharge
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 534
Publication Number: 534.2979
Publication Number: 534.2979

Eli Zettler (he/him/his)
Medical Student
Robert Larner, M.D., College of Medicine at the University of Vermont
Burlington, Vermont, United States
Presenting Author(s)
Background: The provision of intensive care for infants born at 22 and 23 weeks of gestation has become commonplace in some centers in recent years. Although the unique inpatient needs of infants born at 22 and 23 weeks of gestation are distinguished from those of more mature extremely preterm infants (EPI; 24- < 28 weeks), few high-quality sources have examined differences in outpatient needs, including use of health care services, following hospital discharge.
Objective: The purpose of this retrospective cohort study was to assess, among a cohort of EPIs who receive care in a tertiary academic children’s hospital, use of health care services over the first 2 years postnatal.
Design/Methods: Retrospective cohort study conducted at a large, academic children’s hospital (2014 – 2019). Our primary outcome was the number of health care encounters over the first 2 years postnatal. Outpatient health care services were subcategorized as follows: emergency department (ED) usage resulting in admission, ED usage not resulting in admission, outpatient therapy (including occupational, physical, and speech therapies), specialist and/or non-primary care visits, and not otherwise specified. Admission for intensive care was used as a marker for the development of a life-threatening condition.
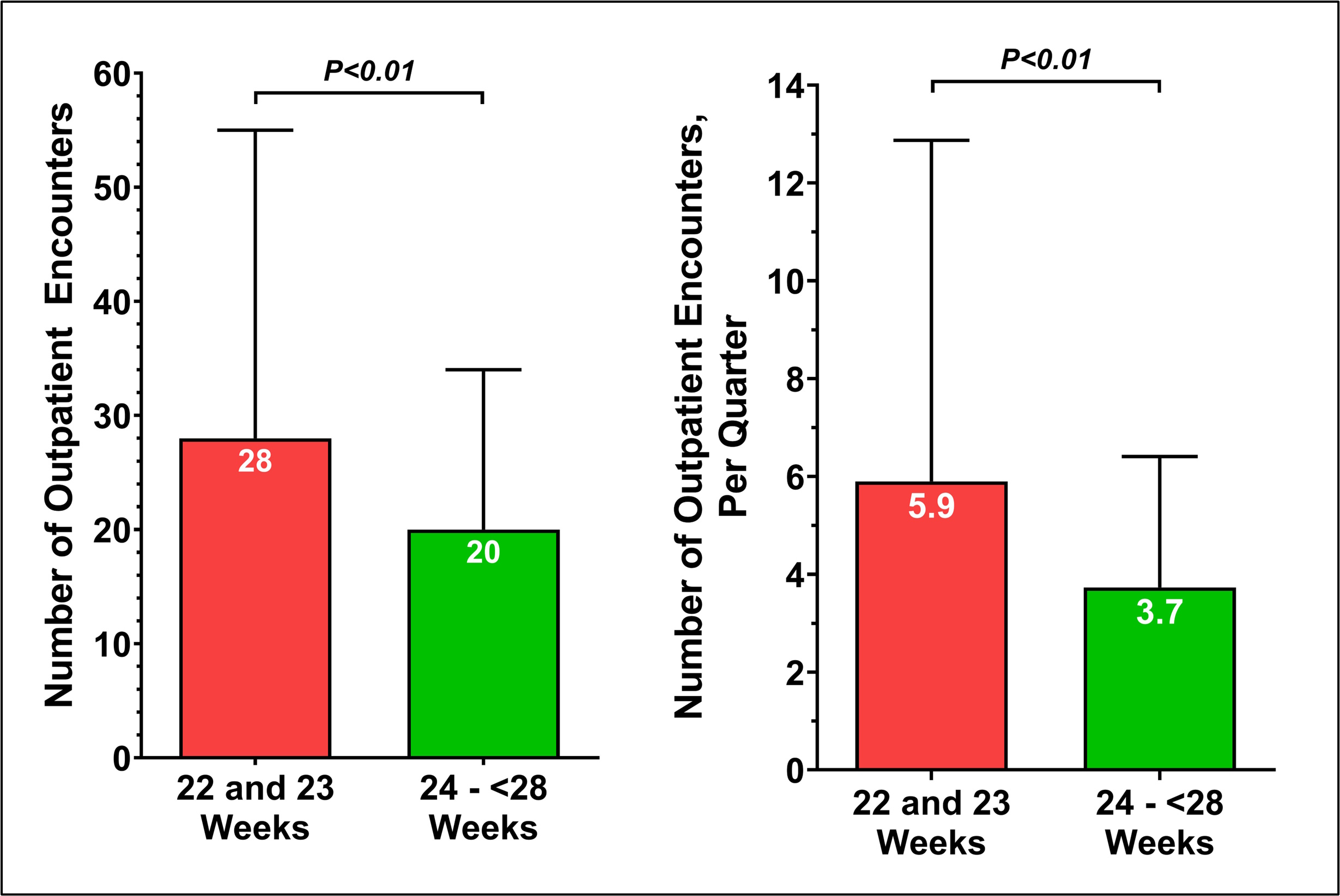
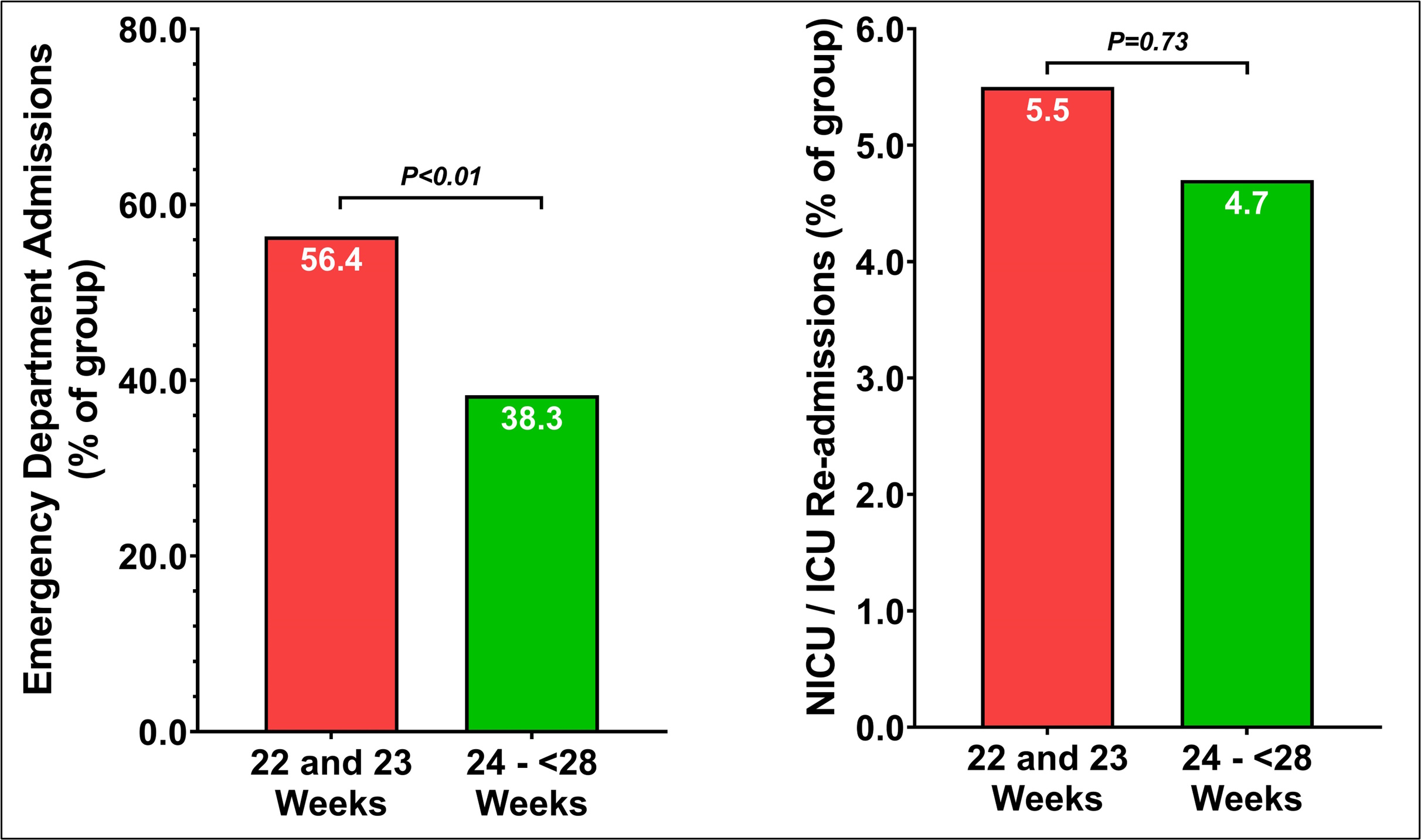
Results: We identified 311 EPI infants during the study period, including 55 born at 22 and 23 weeks of gestation. The median number of outpatient health care encounters for former EPI was 21, (IQR 14-36). Children born at 22 and 23 weeks of gestation had a median of 28 outpatient visits (IQR 16–55), and children born 24-27 6/7 weeks had a median of 20 visits (IQR 13-34; P< 0.01). In the study period, 31 (56.4%) children born at 22 and 23 weeks of gestation had at least 1 ED visit associated with an inpatient admission. By comparison, 98 (38.3%) children born at 24-276 weeks had at least 1 ED visit associated with an inpatient admission. During the study period, 3 (5.5%) children with born at 22 and 23 weeks of gestation had at least 1 ICU admission; by comparison, 12 (4.7%) children 24- 276 weeks had at least 1 ICU admission (p=0.73).
Conclusion(s): An improved understanding of differences in the outpatient health care needs of infants born at 22- and 23-weeks’ gestation compared to more mature EPI provides opportunities for health policy interventions, including the design of a coordinated, multidisciplinary post-discharge care clinic and home visiting service for this at-risk subgroup.