Hospital Medicine
Session: Hospital Medicine 3
340 - Medical Hospitalizations for Children with Mental Health Conditions Before and During the COVID-19 Pandemic
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 340
Publication Number: 340.413
Publication Number: 340.413
.jpg)
Melinda Murphy, MD (she/her/hers)
Associate Professor
USF Health Morsani College of Medicine
Tampa, Florida, United States
Presenting Author(s)
Background: Pediatric hospitalizations for mental health (MH) conditions were increasing both before and early in the pandemic; however, little is known about late-pandemic MH hospitalizations. Children admitted to a medical bed for stabilization of a MH condition may place strain on hospitals which are sub optimally poised to care for them.
Objective: We examined trends in pediatric hospitalization for MH conditions before, during and late-pandemic.
Design/Methods: We examined characteristics of medical hospitalizations with either a primary diagnosis for a MH disorder or a comorbid/secondary MH diagnosis across 43 children’s hospitals using the Pediatric Health Information System. We examined hospitalizations for children ages 5-18 years between 1/18-2/20 (pre-pandemic), 3/20-12/21 (early pandemic), and 1/22-6/23 (late pandemic). We excluded hospitalizations with intensive care unit stays and hospitalizations ending in death. We examined length of stay, 30-day reutilization, and transfers to psychiatric facilities. We used generalized estimating equations to compare outcomes in the pre- and late-pandemic periods accounting for age and severity while clustering on hospital and patient. We also conducted time-series analyses to account for the secular trend in increasing hospitalizations prior to the pandemic, censoring the early pandemic period where pediatric hospital volumes were in flux.
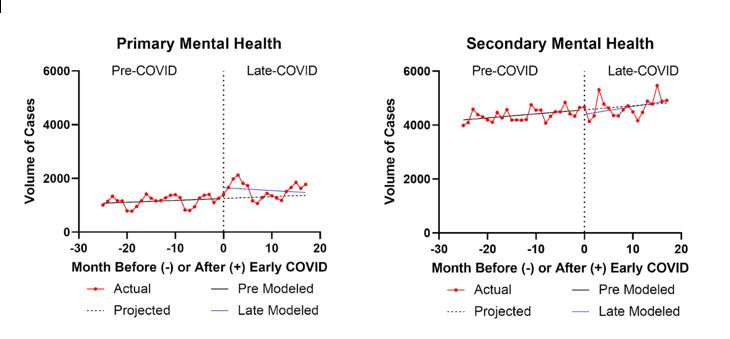
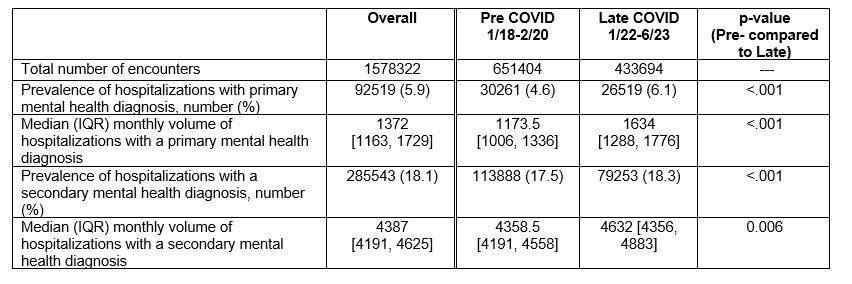
Results: Of the 1,578,322 hospitalizations, 5.9% had a primary MH condition and 18.1% had a secondary MH condition. As a percentage of all hospitalizations, primary MH hospitalizations increased from 4.6% (pre-COVID) to 6.1% (late-COVID); secondary MH increased from 17.5% to 18.3% (Table 1; both p<.001). Monthly volumes for primary MH hospitalizations increased 39.3% from a median of 1173 pre-COVID to a median of 1634 late-COVID (p <.001); hospitalizations with secondary MH diagnoses increased 6.2%. The increase in volumes seen in the late pandemic period followed the pre-pandemic trend (Figure). Characteristics of hospitalizations for primary MH conditions pre- compared to late-pandemic were relatively unchanged except for a significant increase in length of stay from 2.3 to 2.5 days (p=0.039; Table 2).
Conclusion(s): The increase in medical hospitalizations seen pre-pandemic for MH diagnoses has persisted late-pandemic. These findings reiterate the necessity of increased MH resources for children to diagnose and treat these conditions. Further, the increased LOS for children with primary MH conditions may reflect the lack of appropriate facilities for transfer and extended boarding time.
.jpg)