Neonatology
Session: Neonatal Quality Improvement 3
423 - The Development of a Multidisciplinary Gastrostomy Tube Perioperative Care Bundle in the Neonatal Intensive Care Unit Decreases Operative Enteral Access Complications
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 423
Publication Number: 423.2048
Publication Number: 423.2048
- MH
Michelle Hojnicki, DO
Johns Hopkins All Children's Hospital - 501 6th Ave SSt. Petersburg, FL 33701UNITED STATES - St. Pe
Saint Petersburg, Florida, United States
Presenting Author(s)
Background: Gastrostomy tube (G-tube) placement is one of the most common life-sustaining procedures performed in neonatal patients. They provide a safe, long-term access for enteral nutrition. However, complications rates can range from 11-26%. Complications include peristomal leak with skin breakdown, G-tube site infections and G-tube malfunction. Some of these complications can result in increased hospital length or a secondary surgical procedure. Baseline assessment revealed a 30% complication rate within our Neonatal Intensive Care Unit (NICU). We identified the lack of a standardized perioperative care bundle contributing to a large practice variation in perioperative care. We hypothesize that the creation of a bundle in the NICU will decrease operative enteral access complications.
Objective: We sought to create a multidisciplinary perioperative G-tube care bundle to standardize care in our NICU and aimed to reduce perioperative G-tube complications from 30% to 15% in an 18-month period.
Design/Methods: Our cohort included NICU infants who had a surgically placed gastrostomy tube with or without a fundoplication procedure. Patients with percutaneously placed gastrostomy tubes were excluded. The bundle provided guidance from the time of anticipated surgery to 6 weeks post-op or at discharge, whichever came first. The bundle placed emphasis on standardization of G-tube securement from the operating room with a "hashtag taping technique", but also provided guidance for standardization of other components of care including cleaning, pain management and implementation of post-operative feeding.
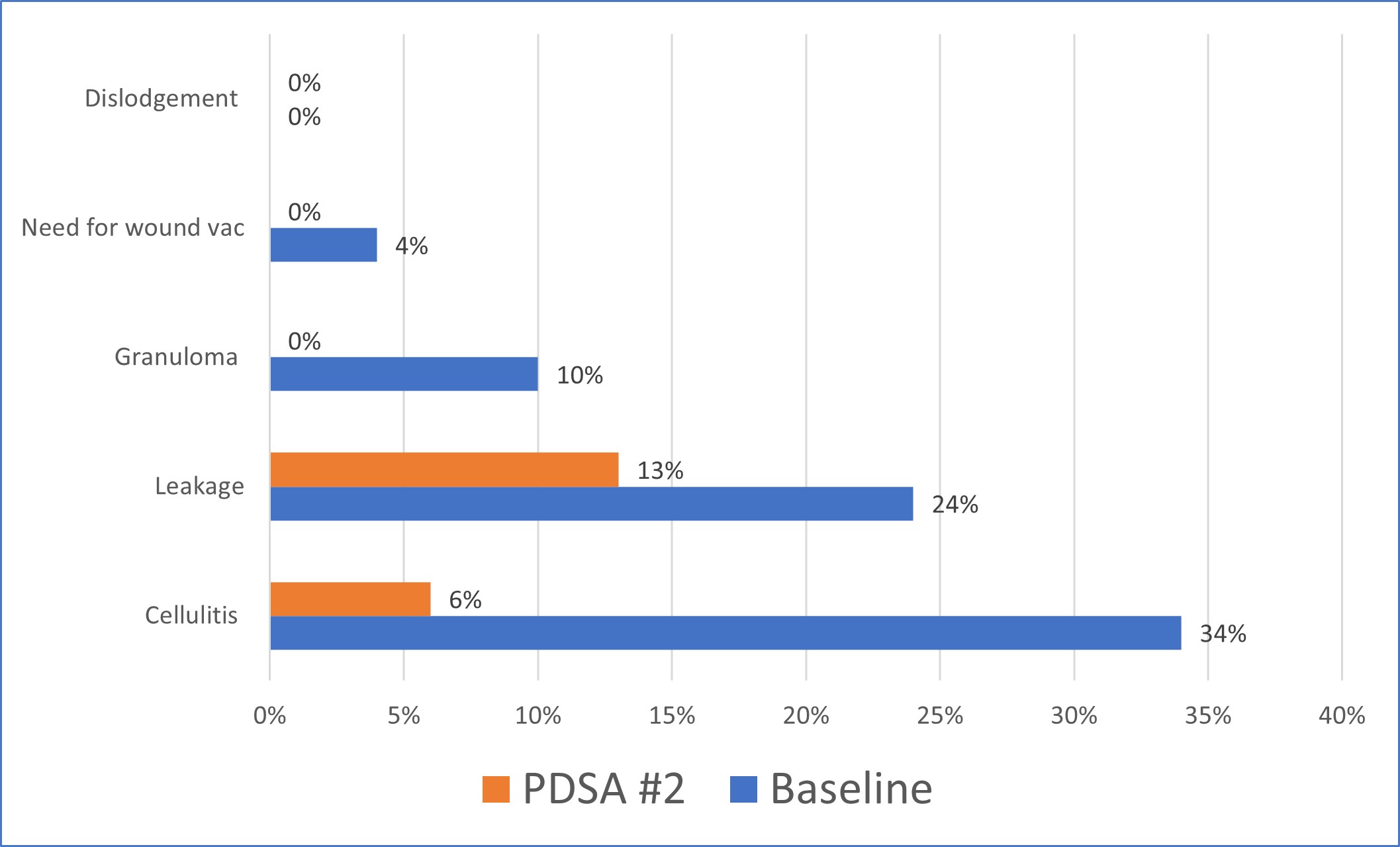
Results: Pre-bundle implementation analysis revealed that most complications were secondary to cellulitis and leakage with several patients requiring wound vac placement for symptom control. The first PDSA cycle, which entailed bundle creation, led to an initial decrease in complications. Further emphasis on standardization of gastrostomy tube securement and nursing education during the second PDSA cycle led to additional improvement and decreased our complication rate down to 17%. Post-operative cellulitis decreased from 34% to 6% and leakage decreased from 24% to 13%. In addition, there were no further cases of patients requiring a wound vac following implementation of the bundle.
Conclusion(s): The creation of a perioperative G-tube care bundle with the collaborative efforts of a multidisciplinary team decreased G-tube related complications from 30 to 17%. Ongoing efforts are underway to disseminate this bundle to other hospital units, and in the outpatient setting and to families for care at home.
.jpg)
.jpg)