Neonatology
Session: Neo-Perinatal Health Care Delivery 3: Epidemiology/Health Services Research
262 - Is Care of Late Preterm Infants in the Mother-Baby Unit Effective?
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 262
Publication Number: 262.2051
Publication Number: 262.2051
.jpg)
Kimberly C. Kullmann, MD, MPH
Resident Physician
Cohen Children's Medical Center
New Hyde Park, New York, United States
Presenting Author(s)
Background: Late preterm infants are at higher risk for morbidities than term infants. To ameliorate these risks by early detection of hypothermia, hypoglycemia, feeding problems, respiratory distress, and other potential complications, our institution’s practice had been to admit all infants born at a gestational age < 36 weeks to the Neonatal Intensive Care Unit (NICU) for observation. To support the mother-infant dyad and promote breastfeeding, we amended our guideline in September 2022 to include direct admission to the Mother-Baby Unit (MBU) for infants born at 35 weeks’ gestation and birth weight > 2000 g.
Objective: The objective of this study was to 1) quantify the impact of this practice change on NICU admissions, 2) characterize the outcomes for infants born at 35 weeks’ gestation admitted directly to the MBU, and 3) compare those outcomes with infants born at 36 weeks’ gestation.
Design/Methods: We conducted a retrospective observational cohort study of infants born at 35-36 weeks’ gestation, comparing those born before (Sept 2021-Sept 2022) and after (Sept 2022-July 2023) the practice change (n=867).
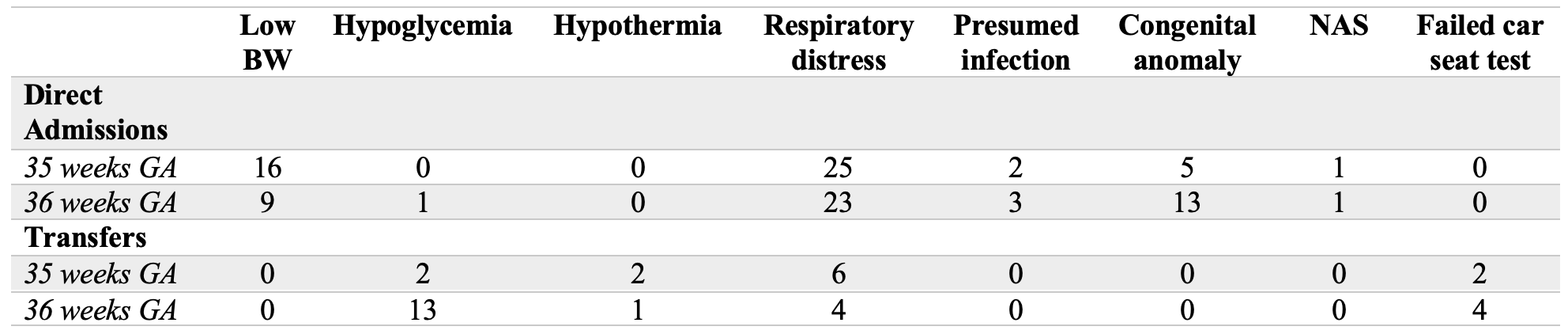
Results: The proportion of total NICU admissions attributable to 35-week infants decreased from 9% before the practice change to 6% after it. Among 35-week infants, admissions to NICU decreased from 100% in the pre-change group to 51% in the post-change group (Table 1). Of those initially admitted to the MBU, 17% later required transfer to the NICU, most commonly for respiratory distress (50%, Table 2). In contrast, 23% and 28% of 36-week infants required admission to the NICU in the pre- and post-change groups, respectively. The most common reason for transfer to NICU for 36-week infants was hypoglycemia (59%).
Conclusion(s): Although initial care in the MBU for infants born at 35 weeks’ gestation and birth weight > 2000 g decreased NICU admissions, almost half of them required NICU care either at birth or thereafter. As the most common cause for NICU transfer was respiratory distress, it is unlikely that additional interventions in the MBU will significantly impact the rate of NICU transfer for a significant subset of 35-week infants. In contrast, only approximately 13% of 36-week infants required NICU care, most frequently for hypoglycemia. Our findings suggest that more rigorous approaches to feeding and thermal management in the MBU may decrease the rate of NICU transfer for 36-week infants.
.png)