Neonatology
Session: Neonatal Quality Improvement 2
408 - The Impact of a Standardized Monitoring and Management Algorithm on Care Practices for Late-Onset Sepsis and Septic Shock in the Neonatal Intensive Care Unit
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 408
Publication Number: 408.2053
Publication Number: 408.2053
- RN
Rema Nagpal, MBBS, MD
Staff
Bharati Vidyapeeth University Medical College, Pune, India
Pune, Maharashtra, India
Presenting Author(s)
Background: Sepsis is a leading cause of adverse outcomes among neonates; however, timely recognition and management of septic shock (defined as the need for vasoactive medications) remain an obstacle. Protocolized sepsis guidelines have been shown to improve sepsis care practices. A Sepsis Monitoring and Management Algorithm was locally developed, and implemented as a part of a large Quality Improvement Plan (QIP) to improve sepsis-related care.
Objective: To assess the impact of the Sepsis Monitoring and Management algorithm on key process and outcome metrics among infants with late-onset sepsis
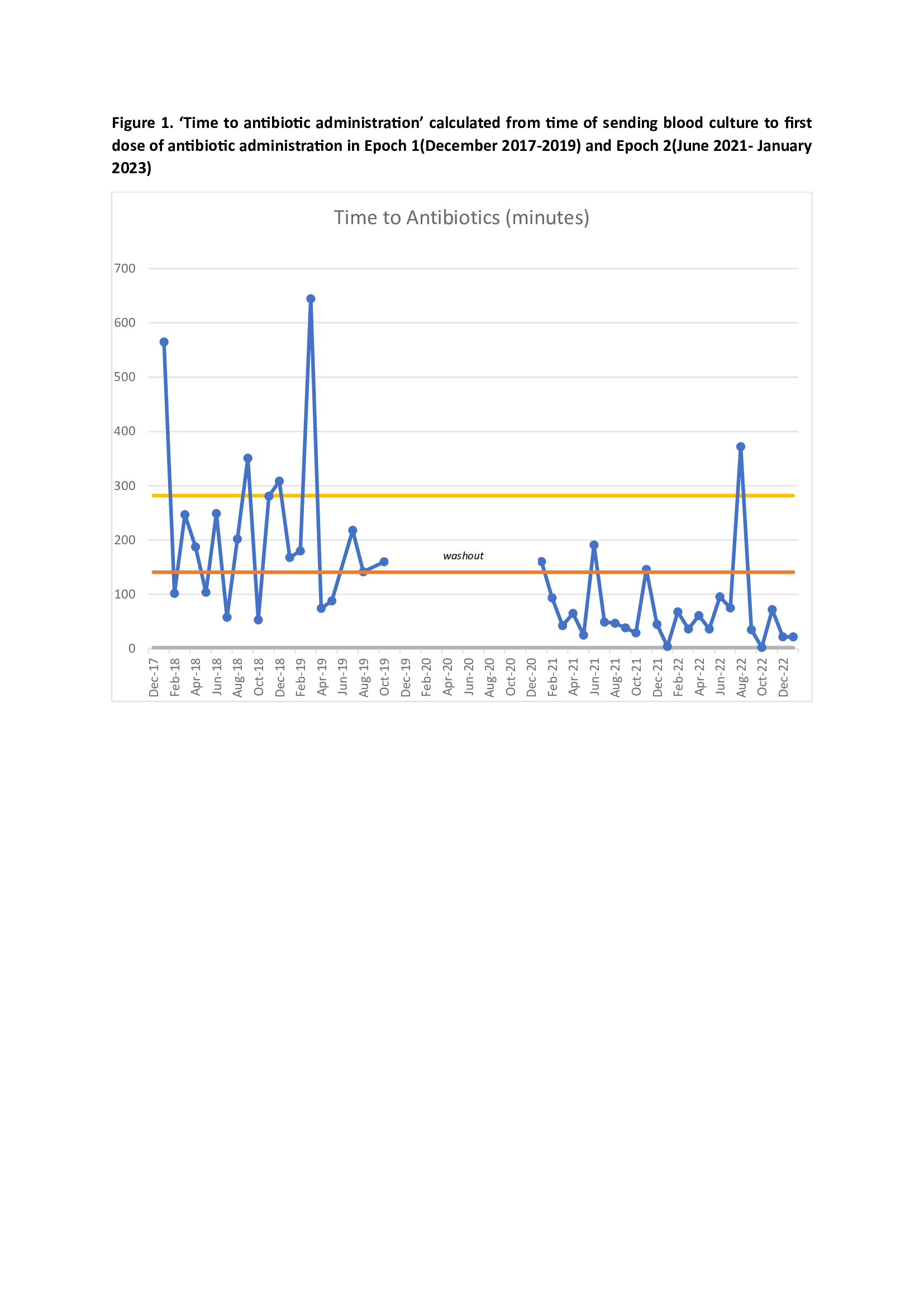
Design/Methods: This single-centre before-after study assessed culture-positive neonates >3 days of age and < 35 weeks gestational age (GA) from two epochs (pre-implementation, Epoch 1: December 2017-19; post, Epoch 2: June 2021- Jan 2023). An 18-month washout period accounted for QIP implementation (unit-wide education, creation of standardized order sets, and algorithm compliance audits) and changes in unit priority due to COVID-19. Baseline demographics, illness severity data, process and outcome metrics were collected, and intergroup comparisons between both epochs were performed. Logistic regression, adjusting for birth GA and weight (BW), sex, small for GA, and total fluid bolus volume given was conducted. Control charts were used to assess for special cause variation.
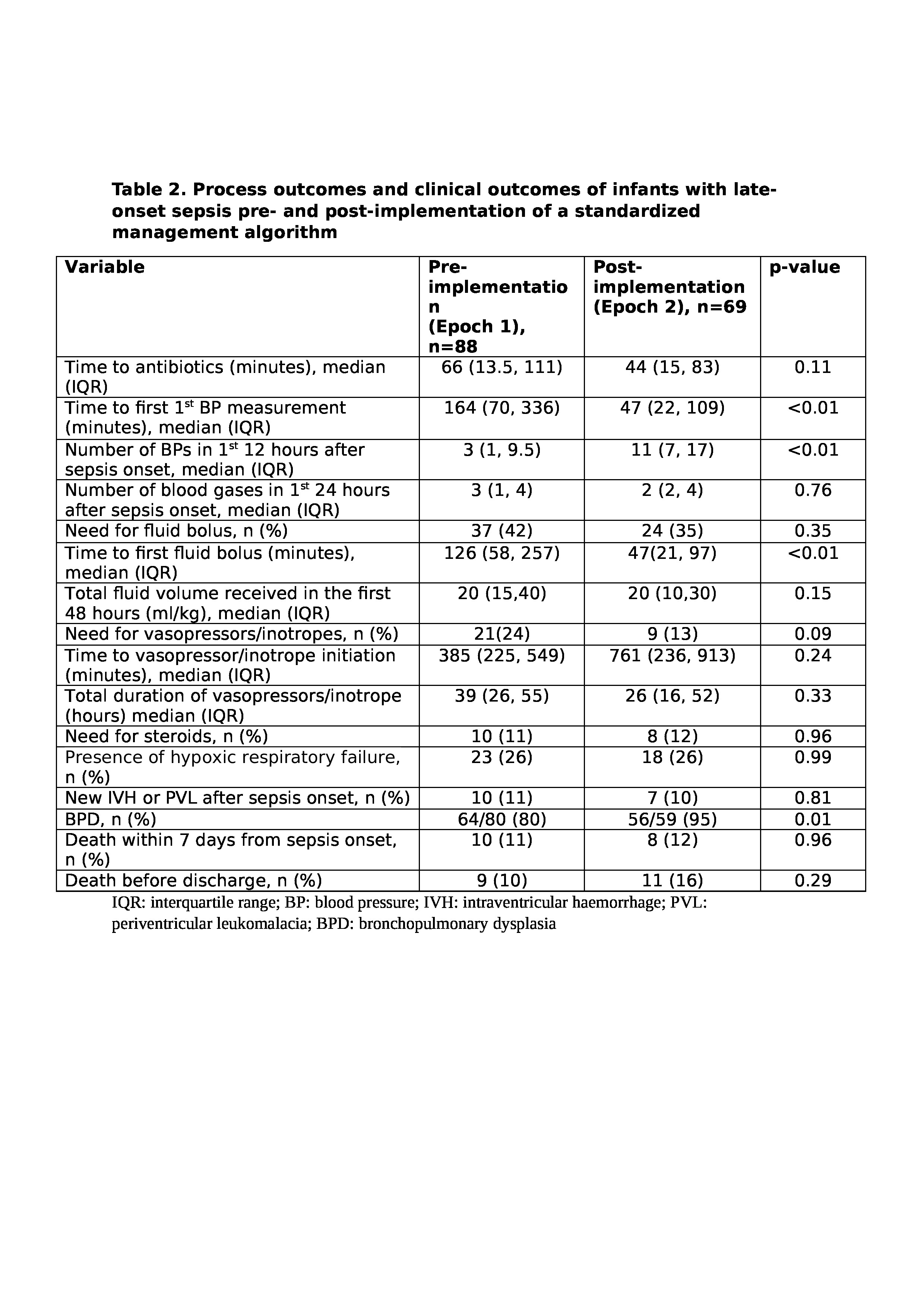
Results: In total, 157 neonates were included, with similar GA and BW between both epochs. In the entire cohort, 30 (19%) infants develop septic shock (Epoch 1: 24%, Epoch 2: 13%). Between the epochs, there were no differences in key antenatal, perinatal, and baseline physiologic illness severity variables (Table 1). Process metrics were improved in the post-implementation epoch, including time to initiation of blood pressure (BP) monitoring after sepsis onset, frequency of BPs taken in the first 12 hours after sepsis onset, and time to first fluid bolus in patients with septic shock (all p-values < 0.01; Table 2). Median time to antibiotics decreased from 66 to 44 minutes (p=0.10; Figure 1). There was no difference in outcome metrics including 7-day mortality (adjusted odds ratio 0.98 [95% confidence interval 0.32, 2.96]), death before discharge (1.67 [0.55, 5.06]), new onset severe IVH (0.85 [0.27, 2.65]). However, BPD among sepsis survivors was higher in Epoch 2 (9.38, [1.53-57.73]).
Conclusion(s): Implementation of a standardized sepsis care algorithm improved sepsis-related processes and care practices; however, in this single centre study, there was no impact on mortality.
.jpg)