Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 1
485 - Risk Factors and Mortality in Infants who Received Bag and Mask Ventilation at Birth: A Secondary Analysis from the Global Network Maternal Newborn Health Registry
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 485
Publication Number: 485.422
Publication Number: 485.422

Zubair H. Aghai, MD (he/him/his)
Professor of Pediatrics
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Birth asphyxia, defined by WHO as a failure to initiate and sustain spontaneous breathing at birth, is one of the leading causes of neonatal deaths worldwide. Infants who failed to establish spontaneous breathing at birth may receive bag and mask ventilation (BMV). Identifying maternal and perinatal risk factors associated with the receipt of BMV at birth using a large database from low- and middle-income countries is a key step in preventing morbidity and mortality associated with birth asphyxia.
Objective: To identify maternal and perinatal risks factors that are associated with the receipt of BMV at birth and compare differences in mortality outcomes of those receiving BMV to those who did not receive BMV at birth using Global Network data from the Maternal Newborn Health Registry.
Design/Methods: This secondary analysis of prospectively collected data from seven sites included fresh stillbirths and live births with BW ≥ 1500 grams. Demographics, clinical characteristics, rates of fresh stillbirth, neonatal mortality (1-28 days) and mortality between 1-42 days were compared between infants who received and did not receive BMV at birth and risk factors for receiving BMV were identified. Relative risk of mortality by BMV was adjusted for region and the propensity score of receiving BMV. Relative variable importance for receiving BMV was calculated using a decision tree model with variance-based feature importance.
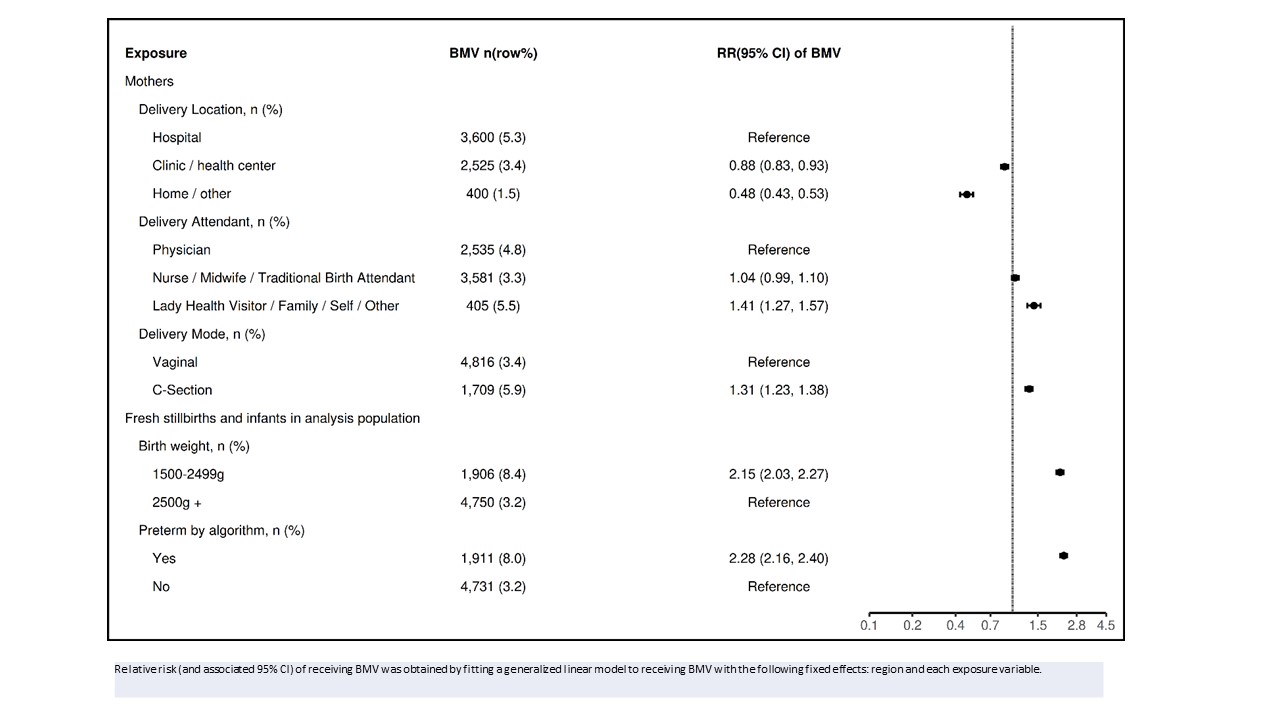
Results: : Between 01/2017 - 04/2023, 171,279 births [6,656 received BMV (3.9%) and 164,623 received no BMV (96.1%)] were included in the analysis [169,439 live births (98.9%) and 1,840 fresh stillbirths (1.1%)]. Risk factors associated with receiving BMV are depicted in Figures 1 & 2. Relative variable importance of receiving BMV included region (100%), maternal education (90%), obstructed/prolonged labor (70%), delivery location (66%) and prematurity (47%). Fresh still birth rate was higher in the BMV group (13.2/1000) compared to No BMV (10.6/1000) but adjusted RR (95% CI) was lower [0.67 (0.54,0.84)]. Neonatal mortality was 185/1000 in the BMV group compared to 11/1000 in the no BMV group. The adjusted RR (95% CI) of neonatal mortality, mortality between 1-42 days and asphyxia as a cause of death for BMV compared to No BMV were 14.23 (13.08,15.49), 12.78 (11.77,13.87) and 2.42 (2.11,2.77), respectively.
Conclusion(s): Early identification of maternal and perinatal factors associated with receiving BMV at birth could enable risk stratification of births. A lower risk for fresh stillbirth among neonates receiving BMV suggests resuscitation is less frequently initiated for fresh stillbirths.
.jpg)
