Neonatology
Session: Neonatal Follow-up 3
531 - Barriers to Neurodevelopmental Follow-Up for NICU Graduates with Severe Bronchopulmonary Dysplasia
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 531
Publication Number: 531.2962
Publication Number: 531.2962
- MR
Michael A. Reisfeld, MD (he/him/his)
Pediatric Fellow
Ann & Robert H. Lurie Children's Hospital of Chicago
Ann and Robert H Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Infants with severe bronchopulmonary dysplasia (sBPD) are at increased risk for neurodevelopmental delays. Completion of outpatient evaluations allows for early detection of developmental impairments and initiation of therapeutic interventions to optimize developmental outcomes.
Objective: To evaluate medical and social factors that may impact rates of completed appointments for infants with sBPD through 18 months of corrected age (CA).
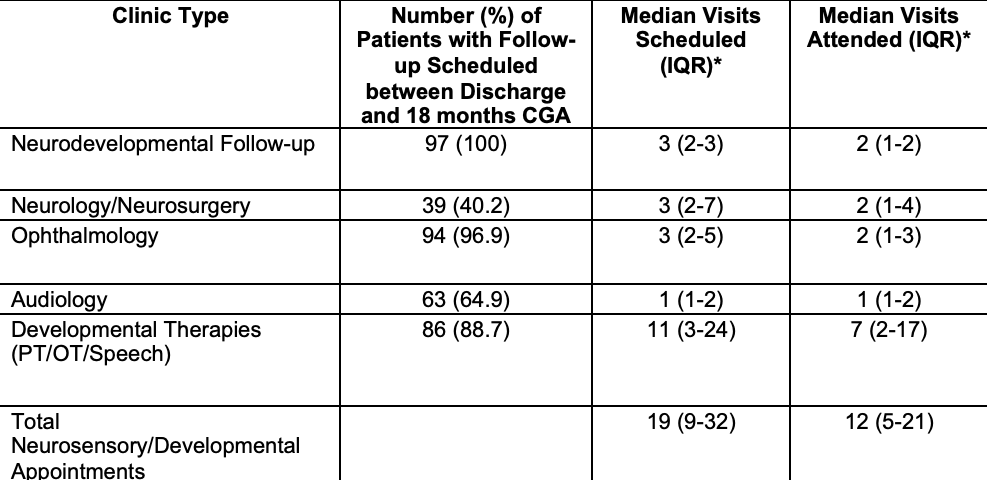
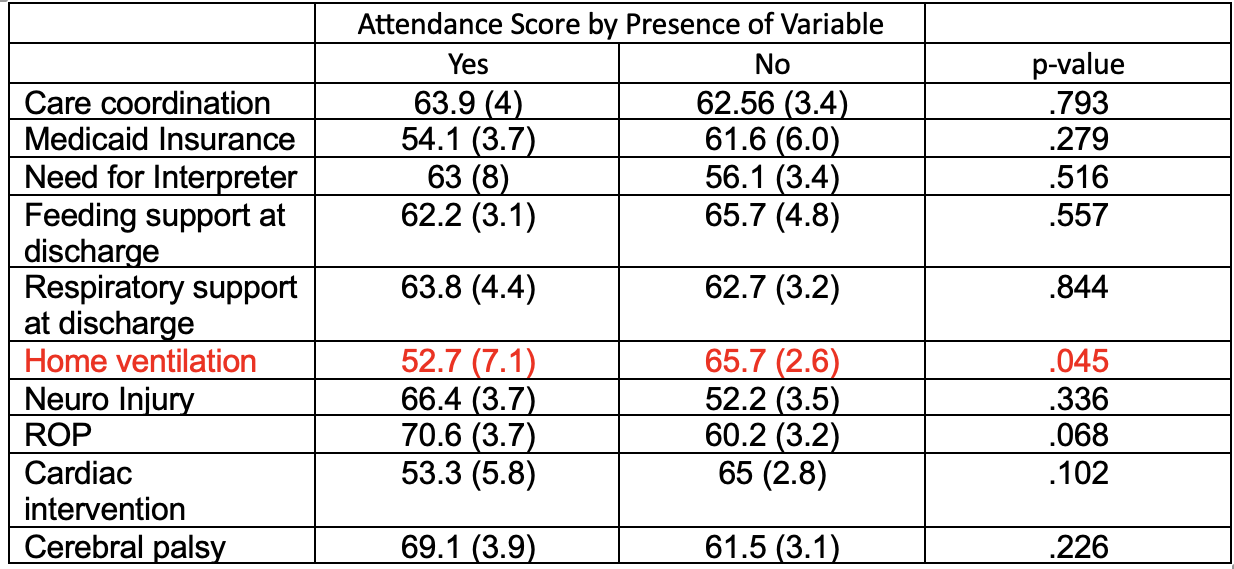
Design/Methods: We included patients born in 2019-21 at < 30 weeks GA admitted to level IV neonatal intensive care unit with sBPD (noninvasive positive pressure or mechanical ventilation at 36 weeks CA), surviving to 18 months CA. Appointments scheduled between discharge and 18 months CA were reviewed in the electronic medical record. Appointments labeled as cancellations or no-shows were considered missed whereas rescheduled appointments were not. Total visits expected included three appointments at neurodevelopmental follow-up clinic (3-6 months, 9-12 months, 15-18 months) as well as all appointments in Neurology/Neurosurgery, Ophthalmology, Audiology, and physical, occupational, and speech therapy. The Attendance Score was defined as the percentage of expected appointments completed. Table 2 shows the medical and social cofactors evaluated and their effect on attendance score.
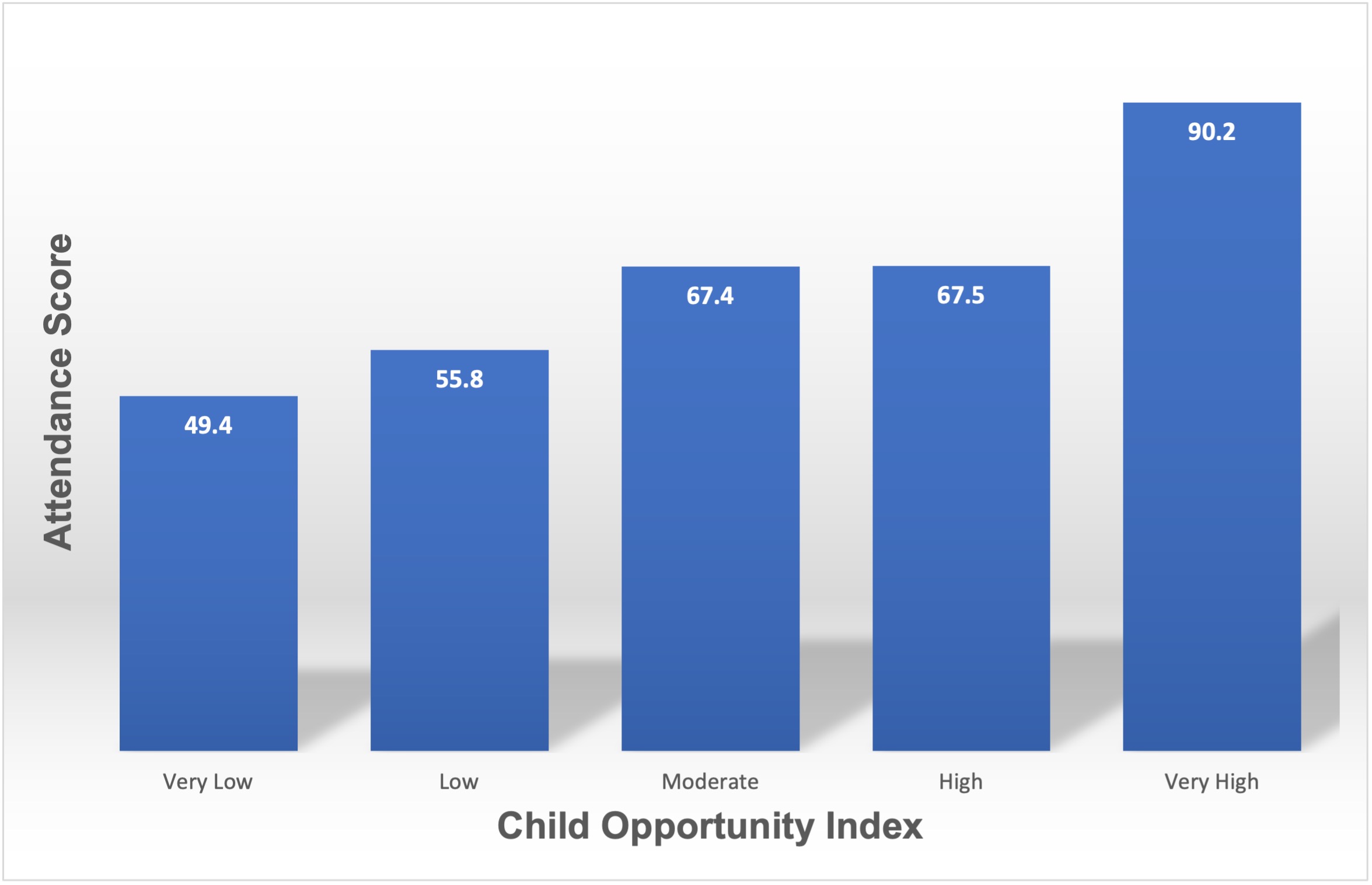
Results: After exclusion of infants discharged to transitional care and those with congenital anomalies, the cohort included 97 patients. The median number of appointments scheduled was 19 (IQR: 9-32). Median attendance score was 65% (IQR: 48-83%). Infants with home mechanical ventilation had lower attendance scores than infants without home ventilation (52.7+31.2%+ vs 65.7+23.4%, p=0.45). Infants with moderate to very high COI had higher attendance scores than infants with low or very low scores (72.4+19.9% vs 51.5%+26.7%, p<.001). No other medical morbidity or social factor was associated with attendance score. In multivariable regression, an attendance score below median of 65% was associated with both home mechanical ventilation (OR 3.85, 95% CI 1.239-11.968) and low-very low COI score (OR 4.517, 95% CI: 1.808-11.286).
Conclusion(s): In this cohort, the degree of medical complexity did not appear to be a significant deterrent to follow-up attendance, with the exception of the need for home ventilation. Association of worsening COI score with decreased attendance suggests social factors may be more relevant driver of clinic attendance. This data may help identify the strongest determinants of follow-up consistency in order to better target interventions to help improve access for our families.