Infectious Diseases
Session: Infectious Diseases 2
76 - Use of Oral Antibiotics for Central Line Associated Bloodstream Infection in Pediatric Cancer and Bone Marrow Transplant Patients
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 76
Publication Number: 76.1291
Publication Number: 76.1291

Darcy Campbell, BA (she/her/hers)
Medical Student
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: Historically, antibiotic treatment for bacteremia has been delivered strictly by the intravenous (IV) route. Literature shows oral (PO) antibiotics not only reach sufficient concentrations to treat bloodstream infections but are also as effective and even safer than IV-only therapy. IV-to-PO switch appears to be less common in immunocompromised patients, despite findings that IV-to-PO switch did not increase morbidity or mortality in adult oncology patients with bacteremia.
Objective: Seattle Children’s Hospital (SCH) established guidelines in 2019 to enable providers to switch antibiotic route from IV to PO in pediatric oncology patients with bacteremia after central line removal (CLR). This retrospective study examines how the likelihood of switch to PO differed by neutropenia status, clinical service, and ICU/non-ICU setting.
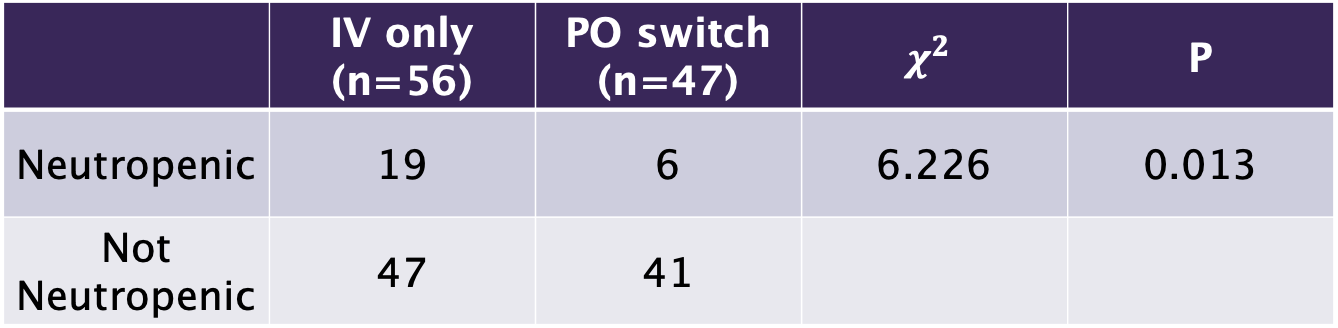
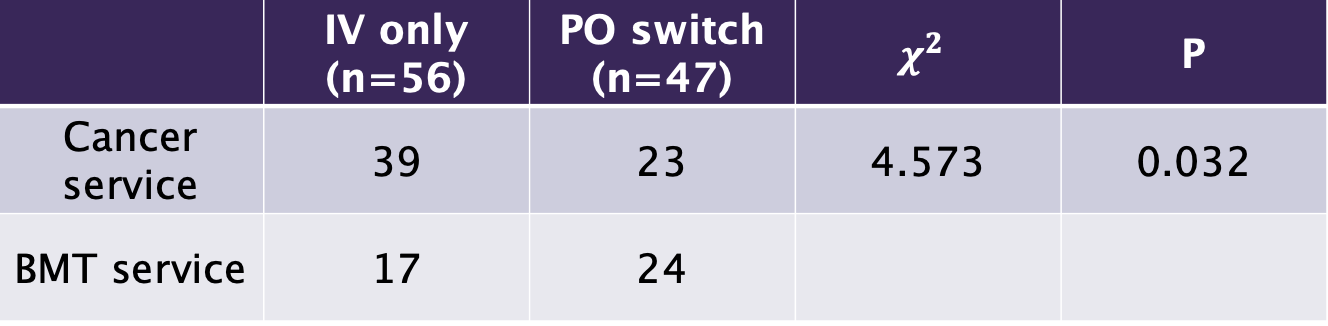
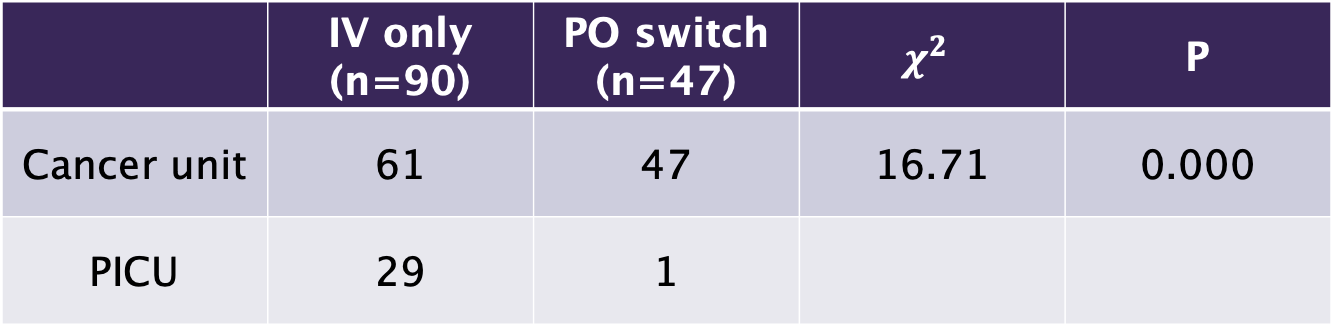
Design/Methods: A retrospective cohort study of hematology/oncology (HONC) and bone marrow transplant (BMT) patients who underwent CLR within 14 days of first positive blood culture was conducted at SCH. The primary outcome was the proportion of patients who underwent IV-to-PO switch. The chi square test was used to compare frequency of IV-to-PO switches between neutropenic vs non-neutropenic patients, HONC and BMT patients, and patients in PICU or not.
Results: We studied 167 episodes of bacteremia with subsequent CLR in 85 patients from October 2020 through September 2023. Overall, 53/167 (31.7%) of CLR episodes resulted in IV-to-PO switch. Neutropenic patients were significantly less likely to be switched to PO antibiotics than non-neutropenic patients. Patients on HONC service were significantly less likely to be switched to PO than patients on BMT service. Patients in the PICU were significantly less likely to be switched to PO than non-PICU patients.
Conclusion(s): After implementation of an IV-to-PO switch protocol for the treatment of bloodstream infection after CLR, 31.7% of eligible patients were converted to enteral therapy. Neutropenic status, clinical service, and PICU status impacted the likelihood of PO switch. Future steps include examining reinfection and mortality outcomes in this population and assessing the impact of race, ethnicity, and language of care on IV-to-PO switch. Although IV-to-PO switch reduces risk of antibiotic toxicity, frequency of IV access, medication cost and IV-associated medical waste, we observed that IV-to-PO switch is underutilized in pediatric HONC and BMT patients after central line removal for bloodstream infection.