Children with Chronic Conditions
Session: Children with Chronic Conditions 2
279 - Prediction of Pediatric Chronic Critical Illness in Infants Admitted to a Level IV Neonatal Intensive Care Unit
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 279
Publication Number: 279.428
Publication Number: 279.428
- SG
Sameer R. Gajjar, MD (he/him/his)
Assistant Professor
University of Texas at Austin Dell Medical School
Austin, Texas, United States
Presenting Author(s)
Background: Improvements in neonatal care have led to a growing population of infants with increasing complexity, chronicity, and fragility, who disproportionately have a higher risk of hospital readmission and utilization of healthcare resources. The definition “pediatric chronic critical illness” (PCCI) was developed to help identify this population.
Objective: In this study, we determined the clinical factors associated with the development of PCCI and the cost of care in infants discharged from a Level IV neonatal intensive care unit (NICU).
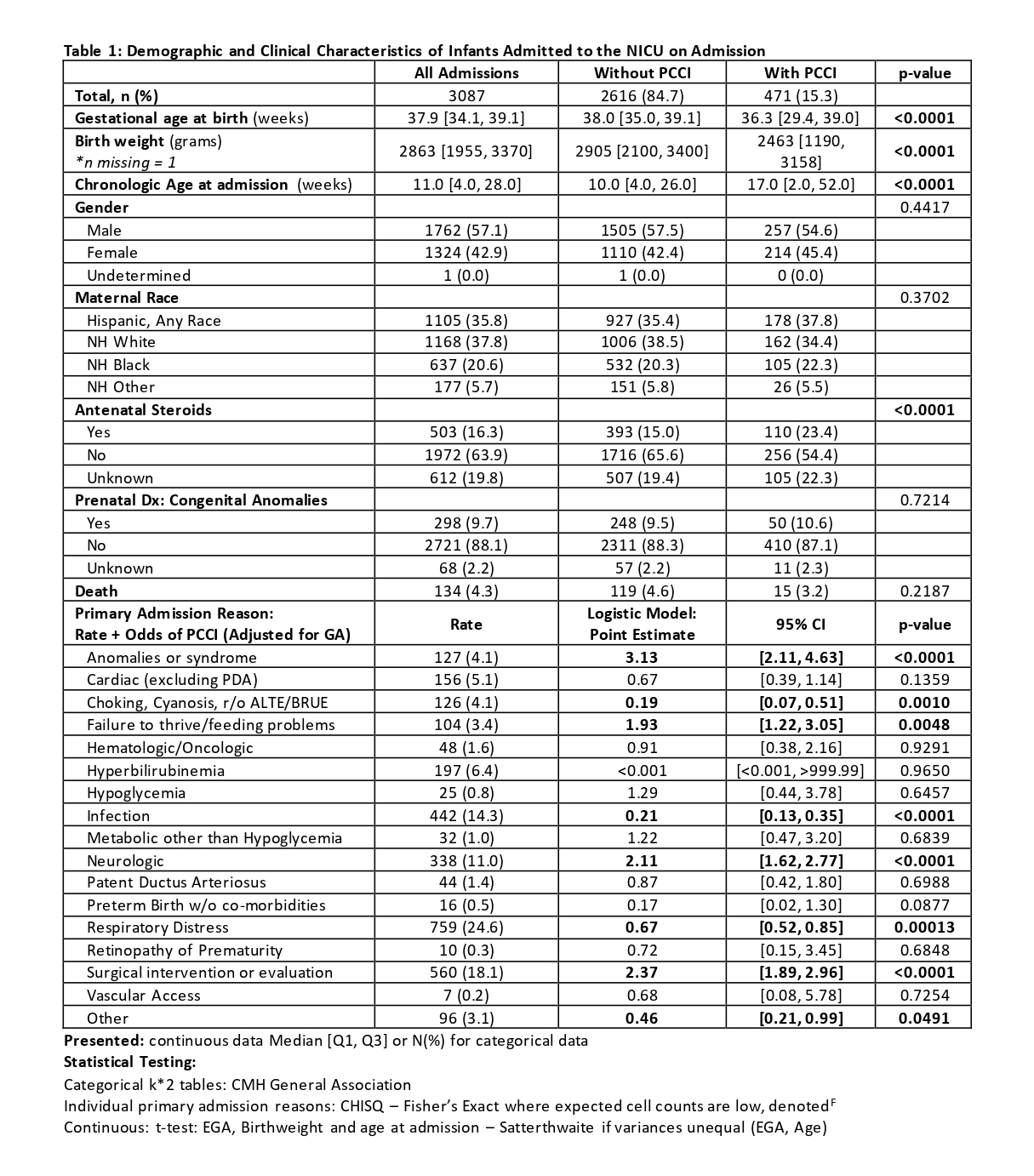
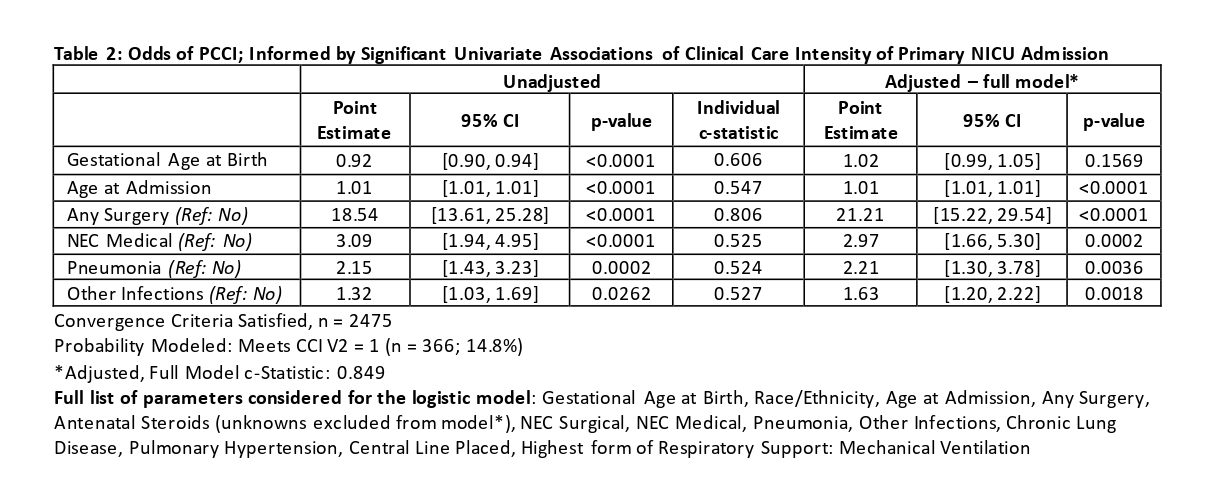
Design/Methods: Retrospective study of all infants admitted to Children’s Medical Center Level IV NICU (Dallas, TX) from 1/1/2011-12/31/2016, using the Children’s Hospital Neonatal Database and the Pediatric Health Information Systems database. Demographic and clinical characteristics were compared between those with and without PCCI. Logistic regression was used to identify those variables independently associated with PCCI (p < 0.05).
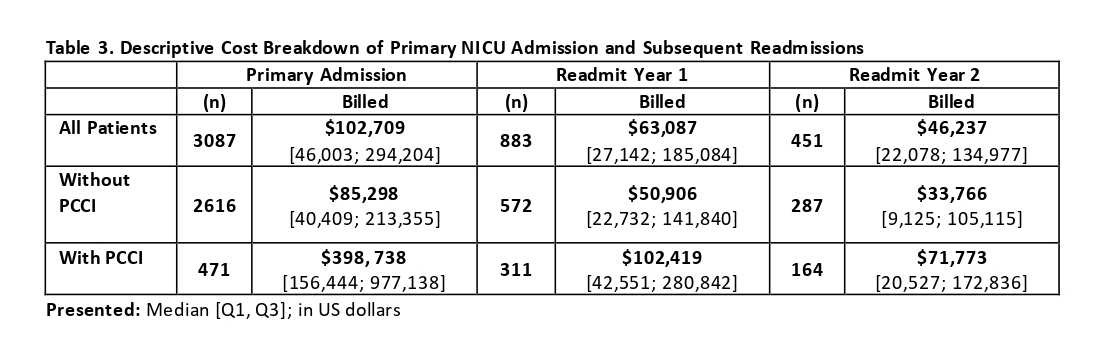
Results: In the study cohort (n=3087), 471 (15.3%) met the criteria for neonatal PCCI. These infants were more premature and had lower birth weight, though chronologically older at the time of admission. Infants classified as PCCI were most likely to have been admitted for congenital anomalies/syndromes (OR: 3.13), surgical evaluation (OR: 2.37), or neurologic disorders (OR: 2.11) independent of gestational age at birth (Table 1). Key clinical characteristics that conferred greater odds of PCCI after adjusting for gestational age at birth and age at admission were surgical intervention (OR: 21.21), medical necrotizing enterocolitis (OR: 2.97), and infections (OR: 1.63) – pneumonia (OR:2.21). (model AUC = 0.85; Table 2). All infants with PCCI were discharged with medical technology, with 34% requiring two or more forms of technology. PCCI was associated with higher healthcare resource utilization, with a greater likelihood of readmission. The median hospital billed cost of infants with PCCI was $398,738, over four-fold higher than infants without PCCI (Table 3). In subsequent readmissions, median hospital costs were two-fold higher in infants with PCCI.
Conclusion(s): This is the largest cohort of NICU patients in which the PCCI definition has been evaluated. We identified factors during hospitalization that were associated with the development of increased medical needs, cost, and vulnerability. Surgical intervention posed the most significant risk with a 20-fold odds of PCCI. Improved identification of at-risk infants will help healthcare systems better allocate resources to support patients and appropriately counsel their families.