Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 3
9 - Improving Psychological Safety in the NICU Clinical Learning Environment
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 9
Publication Number: 9.2950
Publication Number: 9.2950

Betty Pham, MD, MS (she/her/hers)
Physician
University of California, San Diego School of Medicine
San Diego, California, United States
Presenting Author(s)
Background: Psychological safety (PS) occurs when learners feel comfortable raising concerns, asking questions, seeking feedback, and admitting mistakes. The hierarchy and traditions in medicine present many barriers to building an environment of PS.
Objective: Our goal for this QI project was to increase PS in the clinical learning environment where Neonatal Fellows and Pediatric/Med-Peds Residents rotate.
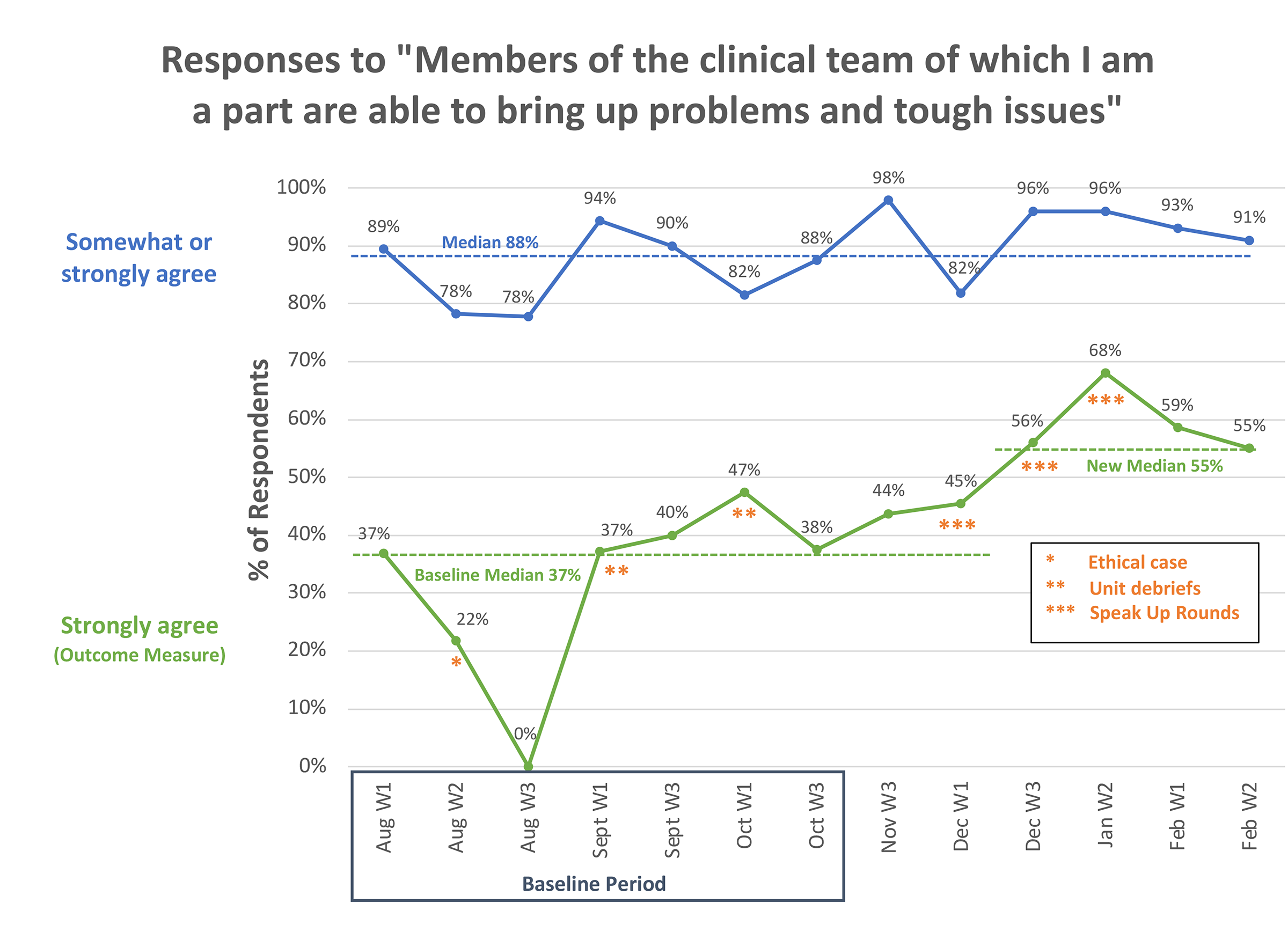
Design/Methods: Staff and learners were surveyed starting August 2022. Our outcome measure of PS was from a validated survey utilizing Likert scale responses (strongly agree to strongly disagree) to, “Members of the clinical team of which I am a part are able to bring up problems and tough issues.” Our SMART aim was to increase the percentage of respondents who strongly agreed with the PS measure by 15% within 7 months (i.e., August 2022 to February 2023). Our process measure was from another validated survey of PS utilizing Likert scale responses (strongly agree to strongly disagree) to, “People in this unit trust each other.” Our balancing measure was the time needed to do interventions to increase PS. A free text field queried, “What can we do to improve the Speak Up (PS) culture?” and data from free text answers were analyzed for themes.
Results: During the baseline period, the median percentage of respondents who strongly agreed with the PS measure was 37%. The median percentage of respondents who strongly/somewhat agreed to the PS measure was high (88%). Common themes highlighted a need to improve involvement of staff on rounds (21%). In response, we implemented, in stepwise PDSA cycles, “Speak Up” team rounds (to formalize the process for the family and bedside team to contribute to medical rounds) as the intervention following initial collection of the baseline data. After implementation of Speak Up Team Rounds we noted a special cause variation and median shift for the PS outcome measure to 55%. The process measure of trust tracked closely with the outcome measure.
Conclusion(s): A multidisciplinary QI approach led to an increase of PS in the clinical learning environment. Asking for input from staff and then implementing changes based on their input resulted in effective PDSA cycles because people felt heard and safe to speak up. In addition, surveying every 2 weeks maintained a focus on PS which positively impacted the learning climate. Future directions include further assessment of the balancing measure, formalization of educational materials for families on NICU team member roles and Speak Up Rounds, and implementing a debriefing tool based on another theme identified from our Qualtrics surveys.