Neonatology
Session: Neonatal Quality Improvement 5
86 - Reducing Unplanned Extubations after Moving to a Single-Family Room NICU
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 86
Publication Number: 86.2937
Publication Number: 86.2937

Cherrie F( Welch, MD MPH
Professor
Wake Forest Baptist Health - Brenner Children's Hospital
Winston Salem, North Carolina, United States
Presenting Author(s)
Background: Unplanned extubation (UE) of critically ill infants on mechanical ventilation can be life threatening, The procedure of reintubation causes pain, increases the risk of airway injury, and ventilator associated pneumonia.
UE events result in additional radiographs and blood gas testing. It is estimated that each incident of UE in the neonatal population adds $36,692 to the cost of care and increases the length of stay by 6.5 days.
After moving from an open ward style NICU to a single-family room NICU and onboarding many new staff, we noticed that our UE rate increased.
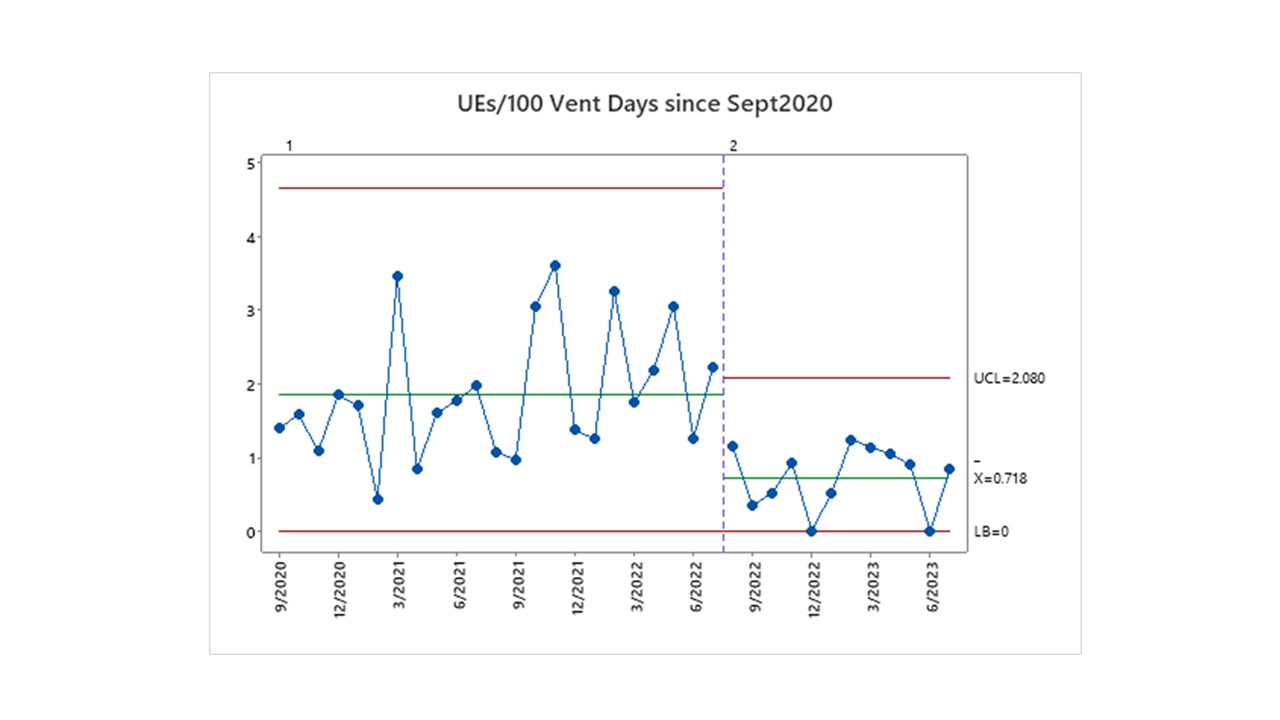
Objective: We sought to reduce our UE rate from 1.8 UE events/100 ventilator days to the national benchmark of less than one UE event per 100 ventilation days.
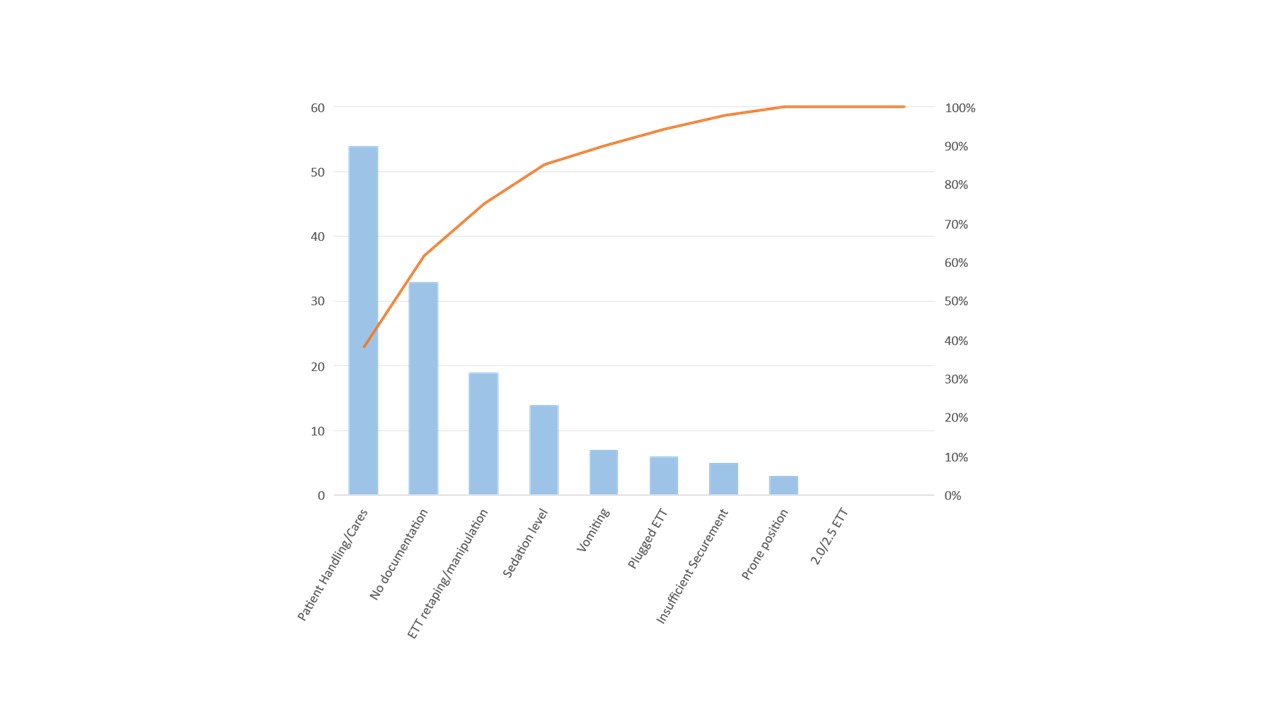
Design/Methods: Having had a successful UE initiative in the past, we reconvened our NICU UE multidisciplinary group and reassessed the current causes of UE in our new unit using a Pareto Chart. We found that many of the same issues, that we had previously addressed, had reemerged and surmised that our previous improvement bundle would likely be effective again given that many new staff had been added and not yet been fully educated on all of the unit’s processes.
The acronym for the UE bundle was “STAMP” and included the following:
• Standardized endotracheal tube securement technique
• Two staff members assist with cares/movement of patients
• A designated “Airway” guardian during movement of patients
• Meeting to debrief after UE events
• Positioning supports for infant’s head, body and ETT/ventilator tubing
We re-educated the staff on the STAMP bundle. In addition, performance feedback was instrumental in gaining by-in from staff regarding the magnitude of our UE problem and to demonstrate the improvements over time from their efforts in following the STAMP bundle. We displayed a timeline of UE events in the staff huddle area to provide our front-line staff with feedback regarding our performance. Each time an UE occurred, a printout of baby footprints was added to the timeline.
Results: As in previous years, we found that our biggest opportunity still involved maintaining the position of the ETT during hands on care of the infant. Therefore, we emphasized the role and importance of the “Airway Guardian” element of our bundle.
Through these efforts, we have been able to reduce the rate of UEs in our new single-family room NICU from 1.8 to 0.7 events/100 vent days.
Conclusion(s): With significant changes, such as onboarding a large number of new staff and moving into a single-family room NICU, quality bundles may need to be revisited and renewed.