Neonatology
Session: Neonatal Fetal Nutrition & Metabolism 2: Fetal/Neonatal Metabolic Dyscrasias
121 - Early postoperative cerebral blood flow and delivery are associated with 2-year neurodevelopmental outcome in infants with d-transposition of the great arteries
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 121
Publication Number: 121.459
Publication Number: 121.459

Anurudhya Karthikeyan, MSc
PhD scholar
Université de Montreal
Montréal, Quebec, Canada
Presenting Author(s)
Background: D-transposition of the great arteries (dTGA) is the 2nd most critical cyanotic congenital heart disease and requires surgery in the first few weeks of age. While corrective surgery has improved survival rates, infants with dTGA are at risk of adverse neurodevelopmental outcomes. The identification of early biomarkers of brain health may help to improve risk stratification and neurodevelopmental outcome.
Objective: To study the associations between early postoperative cerebral metabolic/hemodynamic parameters and 2-year neurodevelopmental outcome in infants with dTGA.
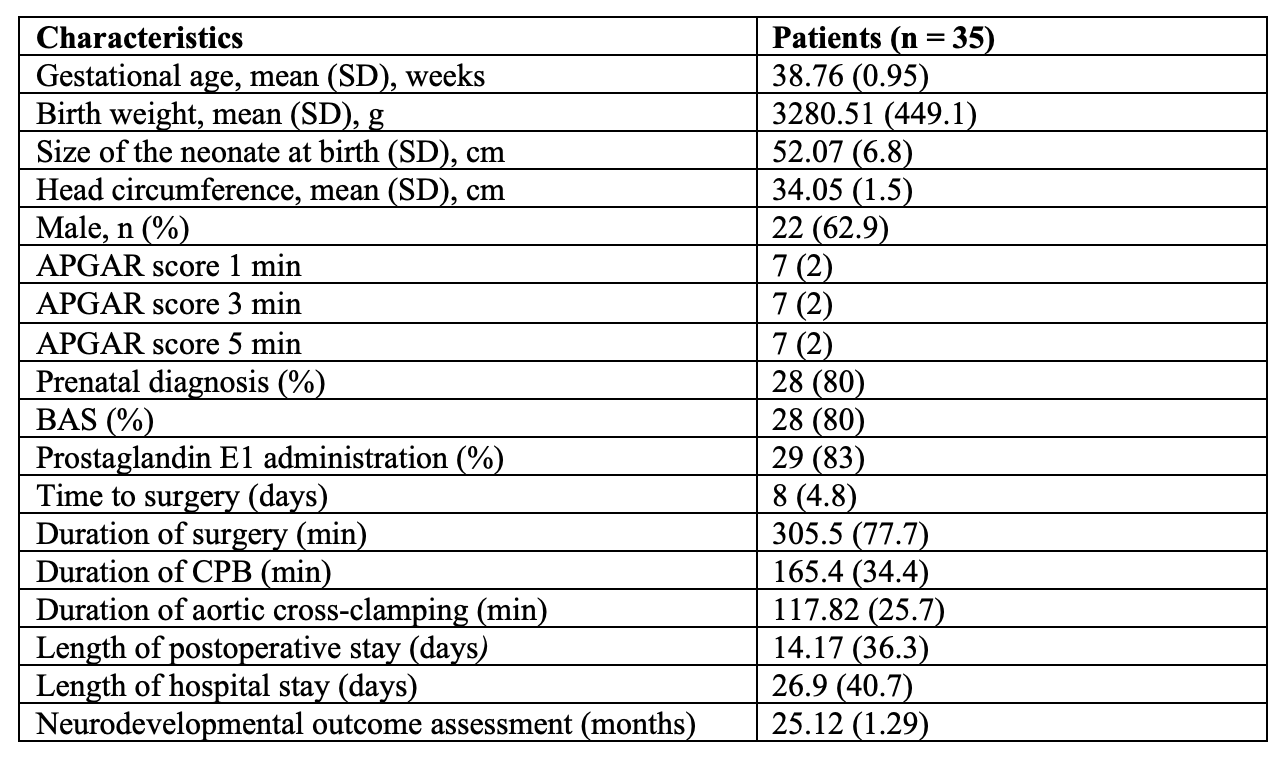
Design/Methods: A single-center prospective observational study including 35 infants with dTGA recruited between 2017 and 2021. Exclusion criteria included infants born prematurely, low birth weight, genetic syndrome, and previous cardiac surgeries. Non-invasive bedside optical neuromonitoring was used to measure cerebral hemoglobin oxygen saturation and an index of microvascular cerebral blood flow (CBFi) during the 72h following the end of aortic cross-clamping. Peripheral arterial oxygen saturation and blood hemoglobin concentration were retrieved from medical charts during this period and used to estimate indices of cerebral oxygen metabolism and delivery (CDO2i). Timepoint measurements were averaged over the 72h period. Neurodevelopmental outcome was assessed at 2 years of age with the Bayley scales of infant and toddler development Ed. III and IV. Spearman’s rank correlation test was used to examine the associations between neuromonitoring parameters and neurodevelopmental scales. Benjamini-Hochberg method was used to correct for multiplicity.
Results: Patient demographics and clinical variables are shown in Table 1. Postoperatively, CBFi and CDO2i were positively associated with both language receptive communication (p=0.048; rho=0.46 and p< 0.001; rho=0.70, respectively) and gross motor (p=0.048; rho=0.46 and p< 0.01; rho=0.54, respectively) scores.
Conclusion(s): Higher cerebral blood flow and delivery in the early postoperative period may reflect a better hemodynamic transition to normal circulation and recovery in infants with dTGA. Their associations with 2-years Bayley scales suggest their potential importance as biomarkers of brain health and neurodevelopment. These results suggest the inclusion of optical neuromonitoring to evaluate early neurodevelopmental risk and as a potential screening tool to assess neuroprotective intervention strategies.