Neonatology
Session: Neonatal Quality Improvement 5
75 - Empowering Families to Define Infant Demographics: An Equity Focused-Quality Improvement Initiative
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 75
Publication Number: 75.2933
Publication Number: 75.2933

Meg Barcroft, DO (she/her/hers)
Neonatal-Perinatal Medicine Fellow + Quality & Safety Fellow
Nationwide Children's Hospital
COLUMBUS, Ohio, United States
Presenting Author(s)
Background: As infant mortality disparities persist nationally, it is paramount that hospitals evaluate local inequities. In Ohio, the mortality of Black infants has remained 2-3x higher than that of White infants for the last decade. With prematurity as the leading cause of statewide infant death, neonatal intensive care units (NICUs) must lead efforts toward health justice. As a first step to assess equitable outcomes, in 2021 our regional NICUs aimed to improve infant race documentation through widespread staff education on editing process. Analysis one year later revealed the third most common race in regional NICUs was Guardian Unavailable to Answer (GUA), a higher distribution from prior.
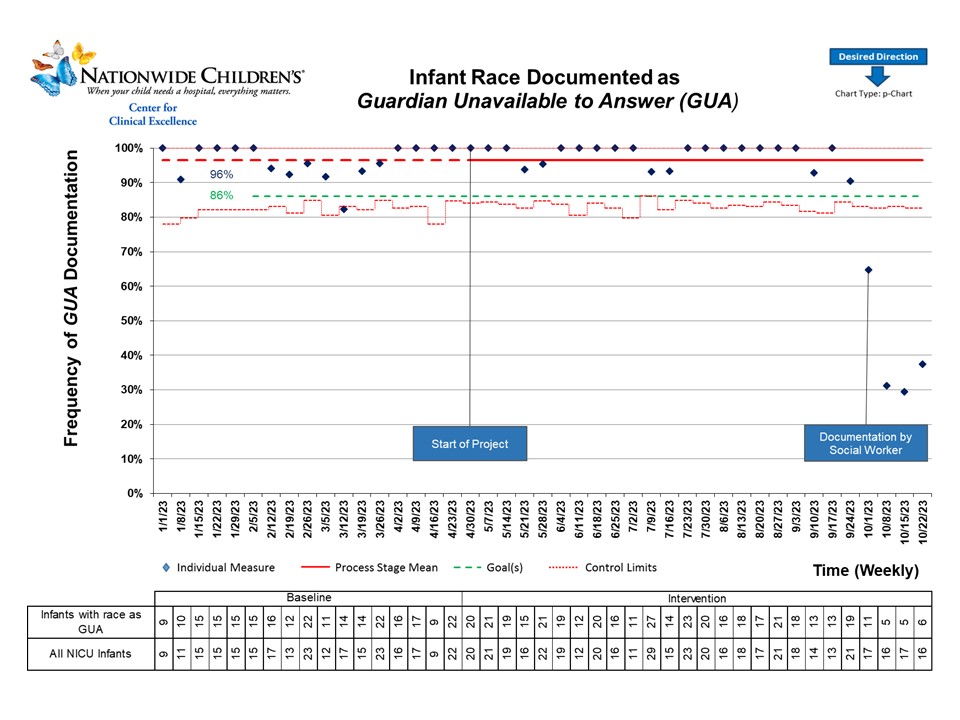
Objective: To decrease infant race documented as GUA at discharge by 10% (96% to 86%) in a level III NICU by December 2023.
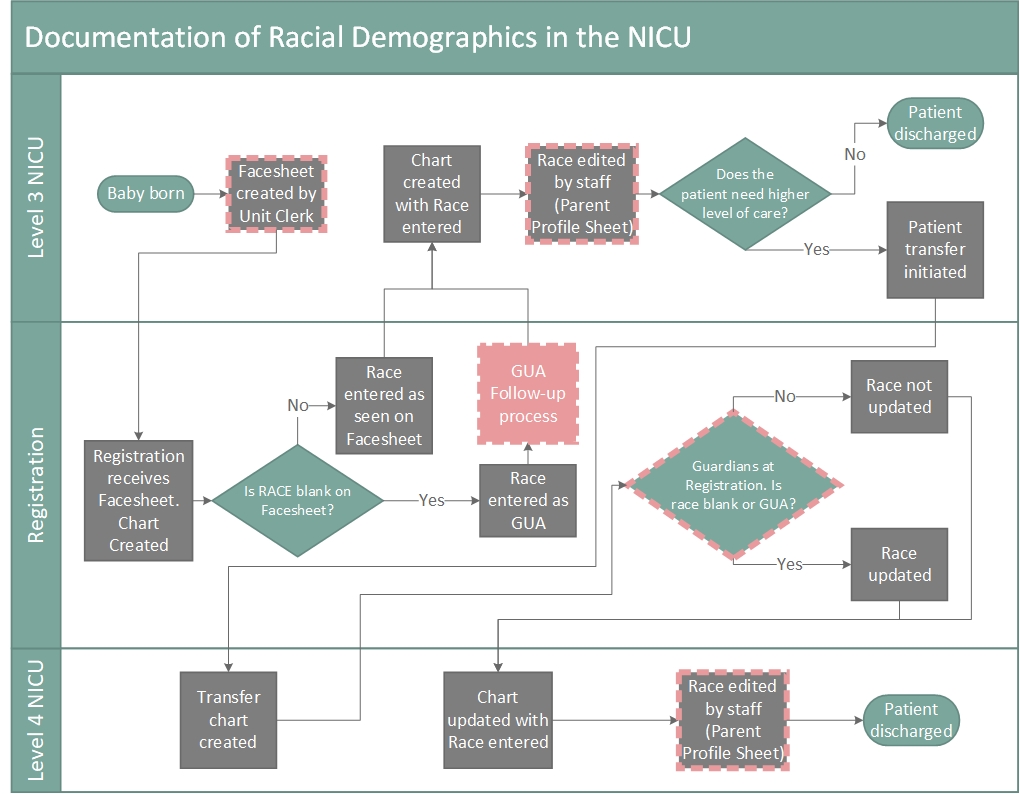
Design/Methods: We developed a multidisciplinary team, completed Gemba walks, and created a complex process map (Figure 1). To empower families to provide the missing demographic data, we conducted Plan-do-study-act (PDSA) cycles including social work assessment and documentation, modification of the hospital-wide patient registration process and staff education. We tracked these as our process measures. Outcome measure was percentage of infant race documented as GUA at discharge. Balancing measures included qualitative feedback on time to document and negative family interactions. We utilized statistical process control methods through a time series design to assess the outcome measure. The project was exempt from IRB review.
Results: Patient characteristics are shown in Table 1. The baseline period rate of GUA documentation was 97%. If infants required a transfer to our Level IV NICU at another location with a different registration process, they had lower rates of GUA documentation at 42%. Following the initial PDSA of social work documentation, there is a trend of decreased GUA documentation in the desired direction to an average of 41% (Figure 2). The social workers performed 83% of the documentation revisions over the four-week period. They reported less than five minutes of documentation time and no negative family interactions.
Conclusion(s): Revising the documentation process of infant race in a level III NICU is feasible. Further investigation in transferred infants revealed a more effective and unique registration process. At our unit level, we continue to refine role delineation and explore methods for direct, family-entered demographic collection. To make systematic, reliable and sustainable changes, we are also revising the registration process.