Neonatology
Session: Neonatal Quality Improvement 1
391 - NO BPD: A Quality Improvement Initiative to Improve the rate of Broncho-Pulmonary Dysplasia(BPD) at a Community level III NICU
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 391
Publication Number: 391.2099
Publication Number: 391.2099

Sneha Taylor, MD (she/her/hers)
Attending Neonatologist
Children's Hospital of Orange County, Orange, CA
Chinohills, California, United States
Presenting Author(s)
Background: Broncho-pulmonary dysplasia (BPD) is the most common complication of prematurity with significant short and long-term consequences. Historically our BPD rates have been comparable to the CPQCC benchmark but inconsistent practices left a lot of room for improvement. A NO BPD QI was initiated in 2020 but was unable to launch until 2021 due to the challenging COVID-19 year of 2020.
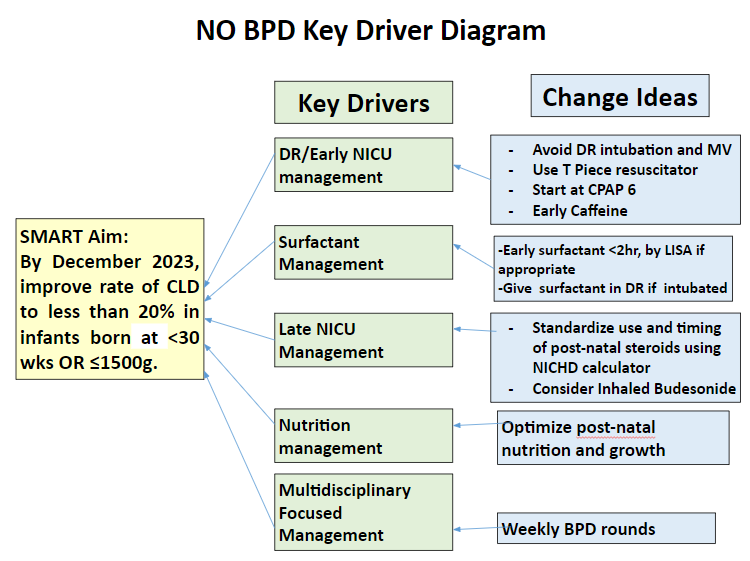
Objective: Improve the rate of BPD defined as oxygen use at 36 weeks PMA to less than 20% by December 2023 for infants born at GA < 30 wks OR ≤1500g by implementing potentially better practices(PBP) using a multidisciplinary approach with standardized care.
Design/Methods: Participants were all CPQCC-eligible inborn and outborn NICU infants born at < 30 wks OR ≤1500g. In 2020, the BPD QI team was created to understand current practices and identify gaps to implement targeted interventions. 2021 PDSA cycle focused on respiratory care in DR and Early NICU care with goals to avoid intubation and mechanical ventilation to maximize CPAP success. Along with it Least Invasive Surfactant Administration technique (LISA) and a separate postnatal growth improvement with better nutrition QI were initiated. 2022 PDSA cycle focused on late NICU respiratory care with a standardized approach to using Post-natal steroids for BPD prevention. 2023 PDSA cycle introduced multidisciplinary weekly BPD rounds for Infants still on respiratory support at 32-34 weeks PMA focusing on optimization of pulmonary function, nutrition, and room air challenge prior to 36 weeks. We measured BPD rate; Pneumothorax rate and Postnatal steroid rate were used as a balancing measure.
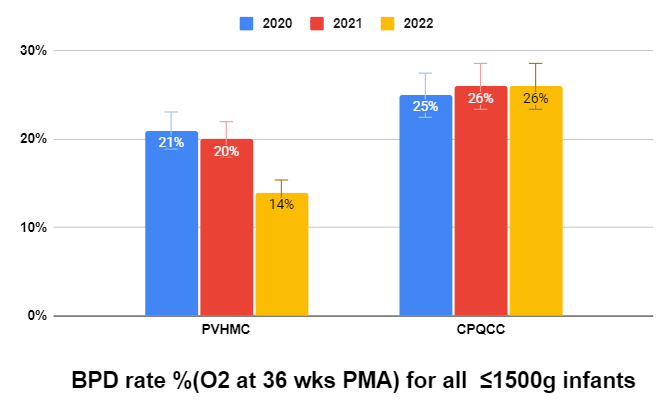
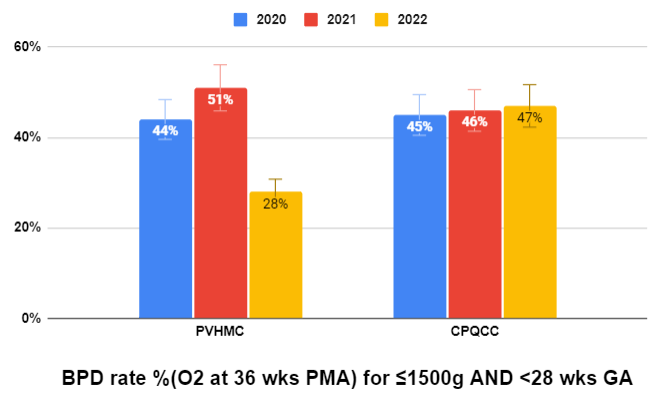
Results: Our BPD rate improved from 21% in 2020 to 14% in 2022 for all infants with ≤1500g BW compared CPQCC benchmark of 26%. Interestingly, our BPD rate has been dramatically improved for infants born < 28wks AND ≤1500g BW from 44% in 2020 to 28% in 2022 compared to CPQCC 47%; and marginally improved for infants born < 30wks AND ≤1500g BW from 28% in 2020 to 26% in 2022 compared to CPQCC 33%. Our Pneumothorax rate has also improved from 5% in 2020 to 1% in 2022 compared to CPQCC's of 3% with Postnatal steroid use rate improving from 13% in 2020 to 8% in 2022 compared to CPQCC's of 15%.
Conclusion(s): BPD is such a multifaceted process making it challenging to implement all potentially better practices with excellent compliance. However, buy-in from all the multidisciplinary team members with great accountability, standardized respiratory and nutritional care, and weekly BPD rounds have made a significant impact on patient outcomes without adverse effects.