Back
Background: Disparities in adult hospitalization outcomes related to race and ethnicity have been reported during the COVID-19 pandemic. It remains unclear what impact the pandemic had on pediatric health disparities for hospitalization outcomes like length of stay (LOS).
Objective: To explore differences in pediatric LOS by race, ethnicity, and language preference pre-COVID-19, during the shutdown, and after reopening.
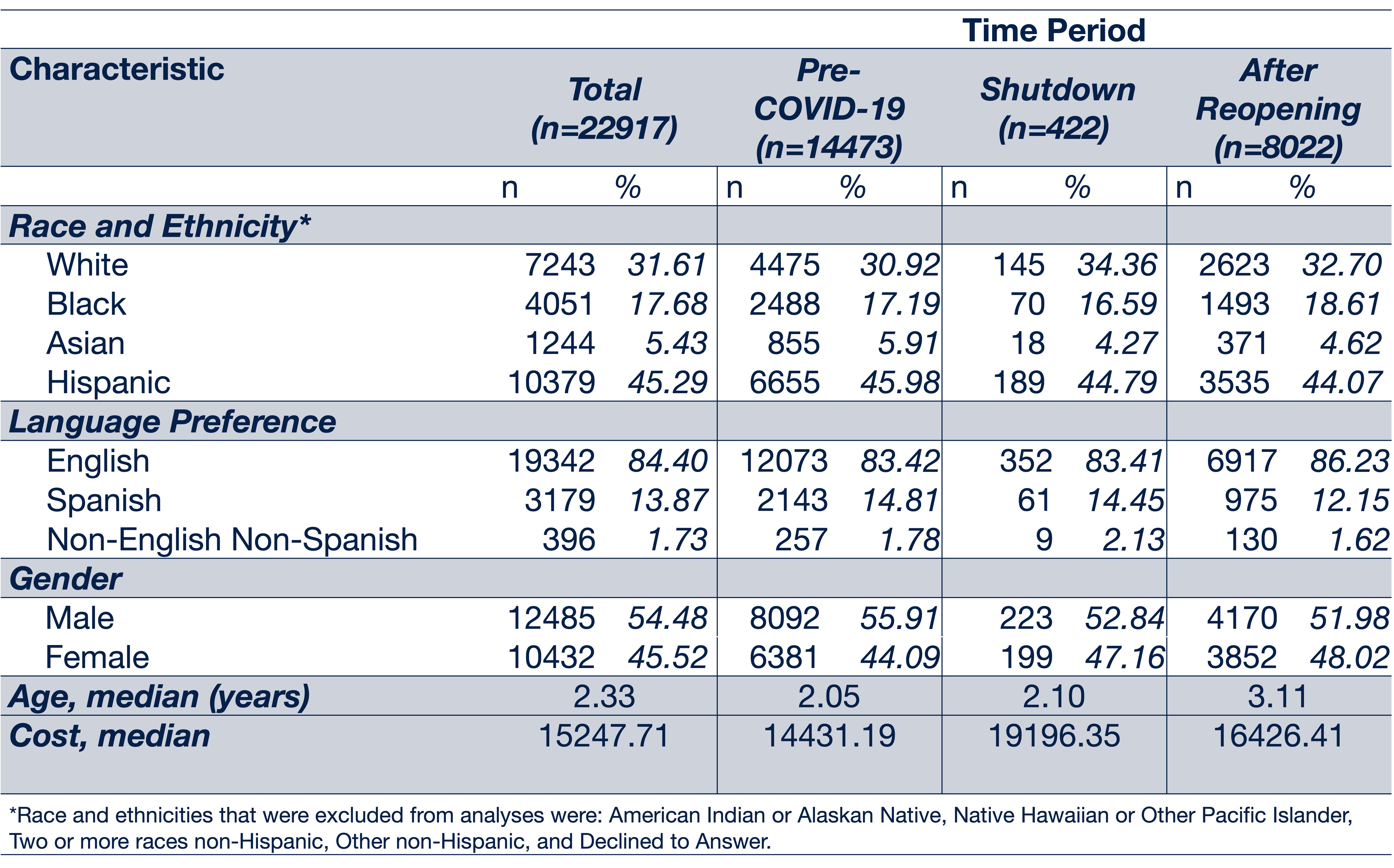
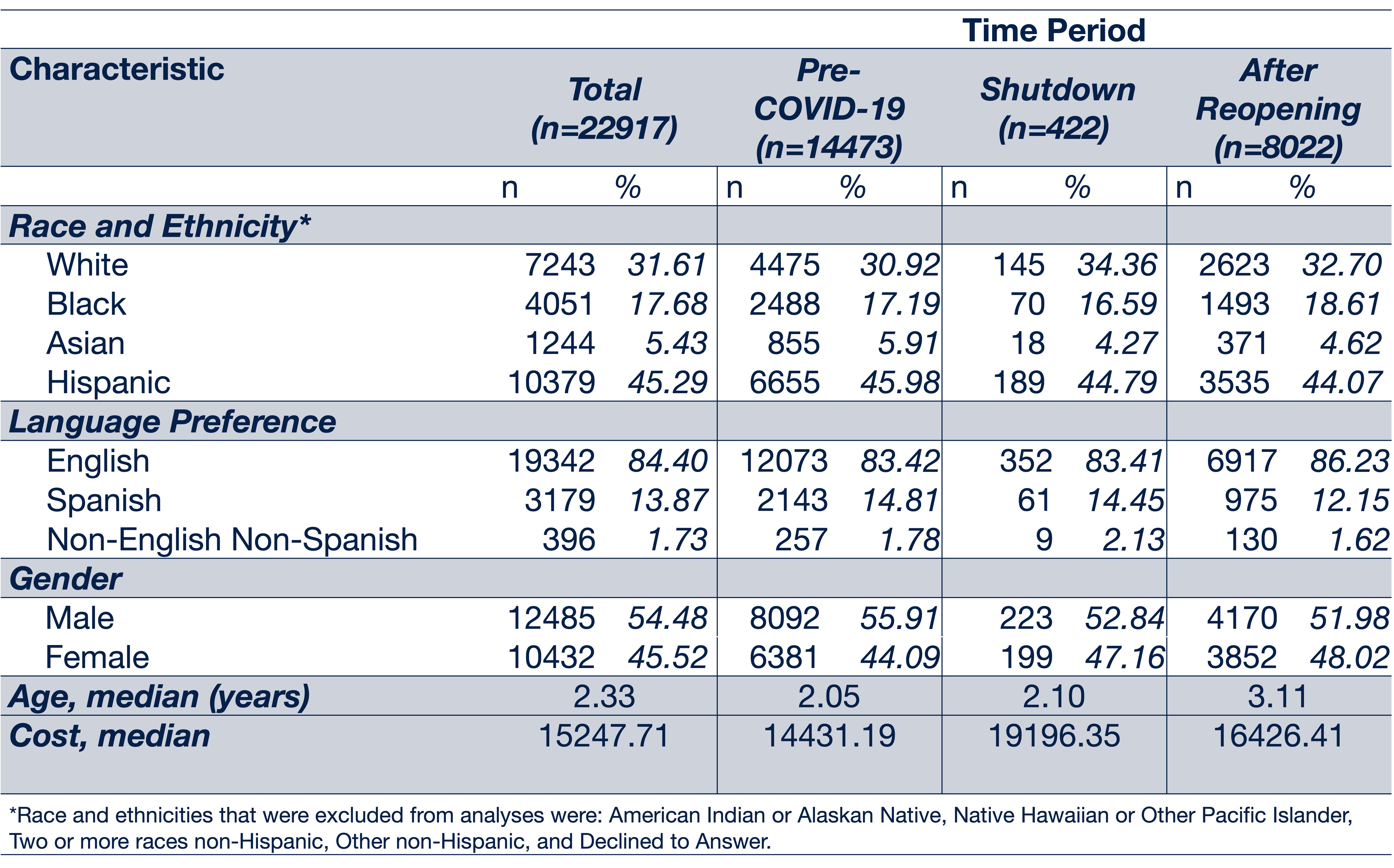
Design/Methods: We obtained electronic health record data for hospitalizations at a quaternary free-standing children’s hospital from Jan. 2017 to Aug. 2022. Inclusion criteria were: age < 18 years old, initial admission to a general pediatrics service for at least one night. Three time periods were examined: pre-COVID-19 (Jan. 2017-Mar. 15, 2020), shutdown (Mar. 16, 2020-May 2020), and after reopening (Jun. 2020-Aug. 2022). Differences in LOS by time period, race/ethnicity, and language were analyzed using simple and multivariate regression models based on a gamma distribution. Analysis of race/ethnicity included: non-Hispanic White, non-Hispanic Black, Asian, Hispanic. Additional data on hospital admission, cost, mortality, ICU transfer, and readmission are undergoing analysis.
Results: There were 22,197 patient encounters (Table 1). Using White patients as the reference group, Black patients had 1.42 times longer LOS pre-COVID-19 (p < .001). For Asian patients pre-COVID-19, LOS was 1.31 times longer (p < .001). For Hispanic patients, there were no statistical differences in LOS. After reopening, Black patients had 1.44 times longer LOS (p < .001), and there were no statistical differences for other races and ethnicities. Using English patients as the reference group, Non-English Non-Spanish (NENS) language preference patients’ LOS was 2.05 times longer pre-COVID-19 (p < .001), with no statistical difference for Spanish language preference. After reopening, NENS language preference patients had no statistical difference in LOS, but Spanish language preference patients had 1.21 times longer LOS (p < .01). During the shutdown, there were no statistical differences in LOS for any race, ethnicity, or language (Table 2).
Conclusion(s): This study found significant disparities in hospital length of stay related to race and language both pre-COVID-19 and after reopening. This may represent the complex interplay of social influencers of health and structural racism with other clinical and non-clinical factors that contribute to healthcare quality and safety, which was masked during the shutdown. Further epidemiologic and solution-oriented research is needed to better understand and address these disparities.
.png)
Hospital Medicine
Session: Hospital Medicine 5
151 - Disparities in Hospital Length of Stay by Race, Ethnicity, and Language: Comparing Pre-COVID-19, Shutdown, and Reopening Periods
Saturday, May 4, 2024
3:30 PM – 6:00 PM ET
Poster Number: 151
Publication Number: 151.1250
Publication Number: 151.1250

Allison M. Lai, MD, MPH (she/her/hers)
Pediatric Hospital Medicine Fellow
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Disparities in adult hospitalization outcomes related to race and ethnicity have been reported during the COVID-19 pandemic. It remains unclear what impact the pandemic had on pediatric health disparities for hospitalization outcomes like length of stay (LOS).
Objective: To explore differences in pediatric LOS by race, ethnicity, and language preference pre-COVID-19, during the shutdown, and after reopening.
Design/Methods: We obtained electronic health record data for hospitalizations at a quaternary free-standing children’s hospital from Jan. 2017 to Aug. 2022. Inclusion criteria were: age < 18 years old, initial admission to a general pediatrics service for at least one night. Three time periods were examined: pre-COVID-19 (Jan. 2017-Mar. 15, 2020), shutdown (Mar. 16, 2020-May 2020), and after reopening (Jun. 2020-Aug. 2022). Differences in LOS by time period, race/ethnicity, and language were analyzed using simple and multivariate regression models based on a gamma distribution. Analysis of race/ethnicity included: non-Hispanic White, non-Hispanic Black, Asian, Hispanic. Additional data on hospital admission, cost, mortality, ICU transfer, and readmission are undergoing analysis.
Results: There were 22,197 patient encounters (Table 1). Using White patients as the reference group, Black patients had 1.42 times longer LOS pre-COVID-19 (p < .001). For Asian patients pre-COVID-19, LOS was 1.31 times longer (p < .001). For Hispanic patients, there were no statistical differences in LOS. After reopening, Black patients had 1.44 times longer LOS (p < .001), and there were no statistical differences for other races and ethnicities. Using English patients as the reference group, Non-English Non-Spanish (NENS) language preference patients’ LOS was 2.05 times longer pre-COVID-19 (p < .001), with no statistical difference for Spanish language preference. After reopening, NENS language preference patients had no statistical difference in LOS, but Spanish language preference patients had 1.21 times longer LOS (p < .01). During the shutdown, there were no statistical differences in LOS for any race, ethnicity, or language (Table 2).
Conclusion(s): This study found significant disparities in hospital length of stay related to race and language both pre-COVID-19 and after reopening. This may represent the complex interplay of social influencers of health and structural racism with other clinical and non-clinical factors that contribute to healthcare quality and safety, which was masked during the shutdown. Further epidemiologic and solution-oriented research is needed to better understand and address these disparities.
.png)
