Cardiology
Session: Cardiology 2
155 - Elevated Distress, Anxiety, and Depression in Pregnancy after Detection of Non-Single Ventricle Congenital Heart Disease: A Mixed Methods Mental Health Pilot Study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 155
Publication Number: 155.2910
Publication Number: 155.2910
- CH
Caitlin Haxel, MD (she/her/hers)
Pediatric Cardiologist
The University of Vermont Children's Hospital
Burlington, Vermont, United States
Presenting Author(s)
Background: Prenatal diagnosis of single ventricle congenital heart disease (CHD) is associated with elevated levels of psychological distress, anxiety, and depression in pregnant persons. Emerging research is concerning that disruptions in perinatal mental health may adversely affect fetal and neonatal brain size, parental-neonatal bonding, and infant neurodevelopment. Prenatal mental health in non-single ventricle CHD is less well known.
Objective: To assess prenatal mental health in CHD, particularly non-single ventricle CHD.
Design/Methods: This was a mixed methods single center prospective pilot study for pregnant persons who received a new fetal diagnosis of non-single ventricle CHD during September 2022 – May 2023. Patients were eligible for inclusion between 18-32 weeks gestation and enrolled 4-10 weeks following diagnosis. Electronic surveys were completed at 4-week intervals until delivery, and 2- and 6-weeks post-partum. Surveys included nationally standardized mental health symptom measures (perceived stress/distress, anxiety, depression) and sought qualitative patient feedback on diagnosis, counseling, fetal CHD-related challenges, and desired support.
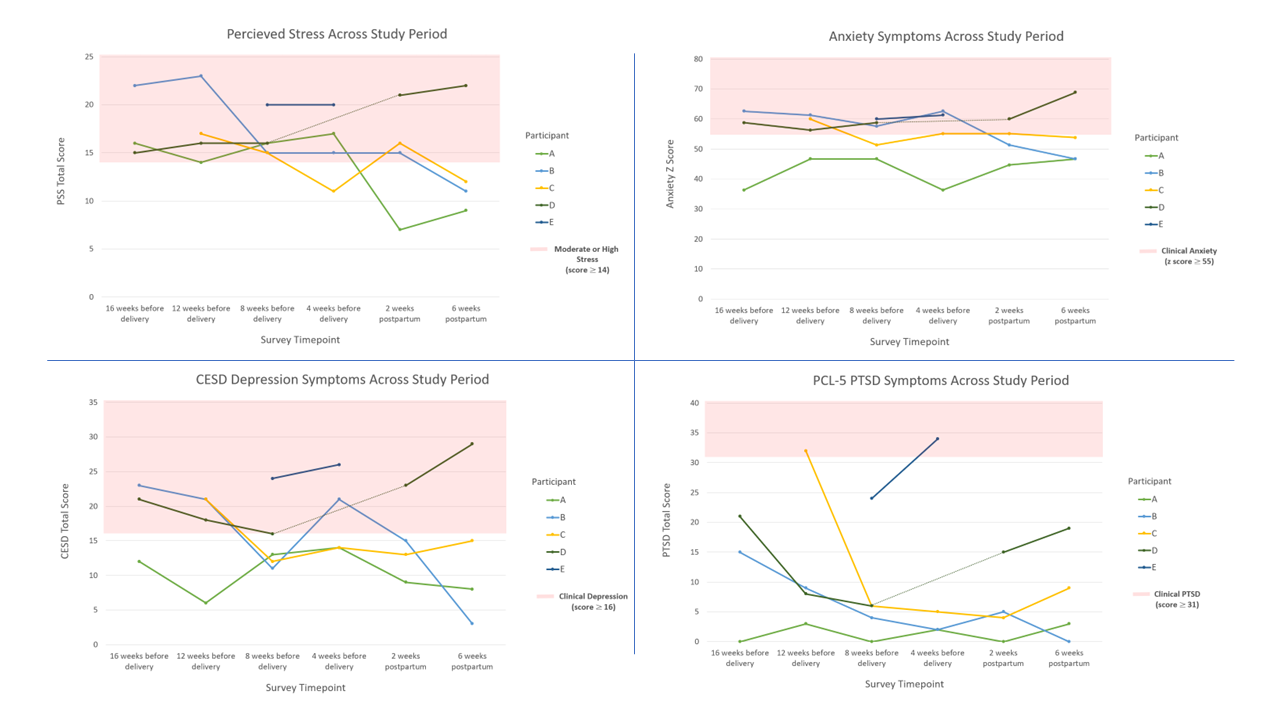
Results: Nine patients (60% eligible) completed surveys. Mean patient age was 32yrs ±7 (range 23-41yrs). CHD diagnoses included right aortic arch (3), coarctation (3), ventricular septal defect (1), atrioventricular canal defect (1) with trisomy 21, and tetralogy of Fallot/pulmonary atresia (1) with trisomy 18. All patients reported clinically elevated acute stress related to a new fetal CHD diagnosis (Impact of Event Scale score ≥9; mean=27.9±10.6). At 4-10 weeks post-diagnosis, clinically elevated symptoms were reported by 8 patients for general stress (Perceived Stress Scale score ≥14; mean=17.7±4.5), 6 patients for anxiety (PROMIS Anxiety Scale Score ≥ 55; mean z-score=55.2±8.7), 5 patients for depression (Center for Epidemiological Studies-Depression Scale score ≥16; mean=16.8±6.8), and 1 patient for post-traumatic stress disorder (PTSD Checklist for DSM-5 score ≥31; mean=13.8±10.5). Symptoms remitted for all but one participant at 6 weeks post-partum (Figure 1).
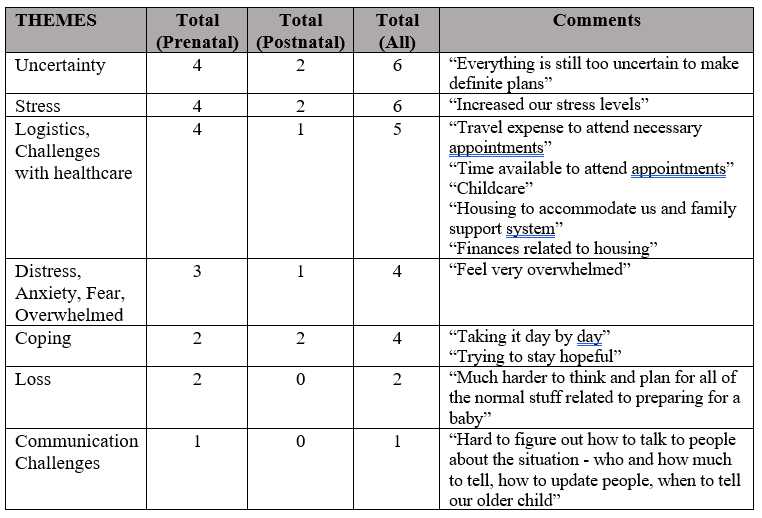
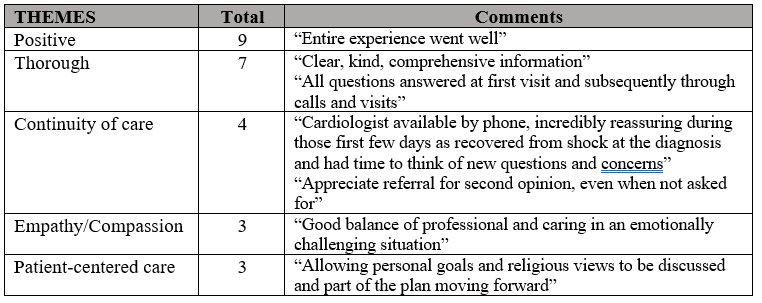
Uncertainty and stress were frequently reported following diagnosis (Table 1). All patients reported a positive initial prenatal counseling experience (Table 2).
Conclusion(s): Pilot data signal clinical concerns for elevated perceived stress, anxiety, and depression after fetal diagnosis of non-single ventricle CHD. Further longitudinal studies surrounding prenatal CHD diagnosis and care could inform counseling approach and support for mental health promotion during pregnancy.