Critical Care
Session: Critical Care 1
108 - Home Discharge from the Pediatric Intensive Care Unit: a Population Cohort
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 108
Publication Number: 108.2908
Publication Number: 108.2908

Nadia Roumeliotis, MD, PhD (she/her/hers)
Pediatric Critical Care Physician
Sainte-Justine University Health Center
Montreal, Quebec, Canada
Presenting Author(s)
Background: Transitions out of ICU have been recognized as a high-risk period for adverse events and increased patient anxiety. Discharge planning, counseling and coordination of follow-up, may be sub-optimal in the PICU compared to the pediatric wards, given the novelty of the practice, the lack of follow-up resources, and relative inexperience with anticipatory guidance. This may increase unplanned return visits. Although adult studies have demonstrated that discharge directly home from the ICU is safe, the prevalence, determinants and safety of discharging children directly home from the PICU has not been established.
Objective: To describe the prevalence and determinants of discharge directly home from the PICU.
Design/Methods: This is a population cohort using the Virtual Pediatric Systems (VPS) dataset of pediatric intensive care admissions in North America between January 1st 2015 and June 30th 2021. Hospitalized children younger than 18 years admitted to a participating PICU, who survived their critical illness and were discharged either home, or to the ward. We excluded patients who were transferred to another PICU, whose discharge disposition was unclear or who were readmitted to PICU. Demographic, PICU admission, and unit characteristics were measured according to discharge disposition. A multivariable logistic regression model was used to evaluate determinants of discharge directly home.
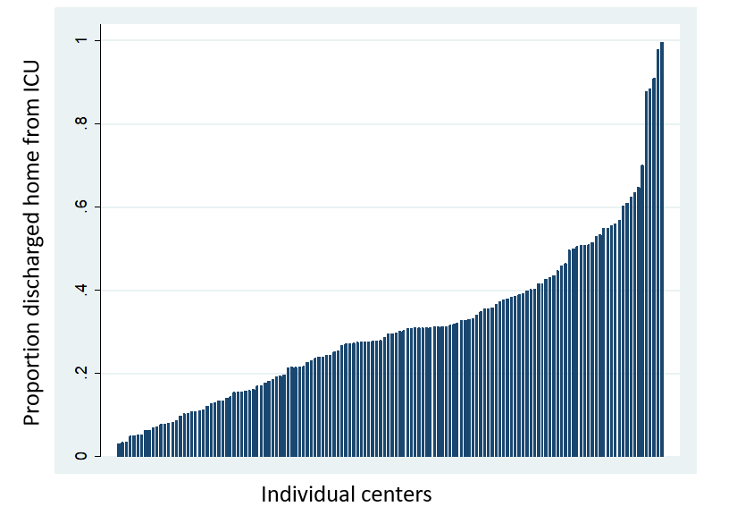
Results: The cohort included 696,442 PICU admissions, of which 173,159 (25%) were discharged directly home. Across sites the proportion of discharge directly home ranged from 0 to 100%. Clinician factors associated with discharge home include age 2-5 years (OR 1.08, 95% CI 1.06-1.10), surgical diagnosis (OR 1.7, 95% CI 1.65-1.75), and scheduled admission (OR 2.7, 95% CI 2.6-2.8). Children with shock and Hematology/Oncology disorders were less likely to be discharged home (OR 0.42, 95% CI 0.41-0.44). The most important factor associated with discharge directly home was previous discharge home (OR 16.14, 95% CI 15.4-16.8). Smaller level 1 units were more likely to discharge directly home (OR 2.55, 95% CI 2.48-2.60), compared to large academic PICUs.
Conclusion(s): One in 4 children is discharged directly home after a PICU admission. While the practice is common, there are selected patients that are more likely to go directly home, like scheduled admissions and surgical diagnoses, however a large variability exists between centres. Given the potential efficiency of the practice in terms of ressources utilization, more research is needed to confirm the safety of discharge directly home from the PICU.