Public Health & Prevention
Session: Public Health & Prevention 3
239 - U.S. Primary Care Pediatricians’ Reported Barriers to Pandemic Preparedness, 2018 vs. 2022
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 239
Publication Number: 239.1221
Publication Number: 239.1221
- CS
Chloe Somberg, BA (she/her/hers)
Research/Database Analyst
American Academy of Pediatrics
Chicago, Illinois, United States
Presenting Author(s)
Background: The COVID-19 pandemic placed enormous strain on pediatric care providers. Having confronted the challenges of a global pandemic, have pediatrician perspectives regarding pandemic preparedness changed?
Objective: Compare US primary care pediatricians’ anticipated barriers to pandemic preparedness before they had experienced such an event to those who had experienced the COVID-19 pandemic. Examine practice characteristics associated with rating multiple barriers to pandemic preparedness as significant barriers in each period.
Design/Methods: We examined primary care pediatricians’ perspectives before COVID-19 (2018) and 2 years after the outbreak of COVID-19 (2022). Comparisons were made drawing on AAP Periodic Surveys in 2018 and 2022. Each survey was a nationally representative sample of non-retired US AAP members (residents excluded). Response rates were 42% in 2018 and 37% in 2022. Data were collected on pediatricians’ assessment of 5 barriers to pandemic preparedness at their practice: significant barrier, moderate barrier, slight barrier, and not a barrier. A combined measure was created using responses across the 5 barriers: multiple (2 or more) significant barriers or not ( < 2). Chi-square tests compared percent of respondents rating each barrier as significant by year to determine if the barriers varied between 2018 and 2022. Multivariable logistic regression examined multiple significant barriers by year, adjusting for core practice characteristics.
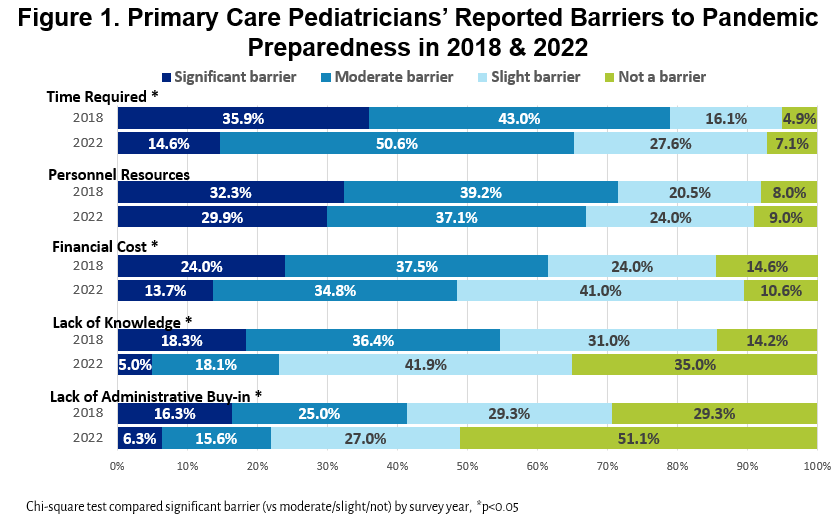
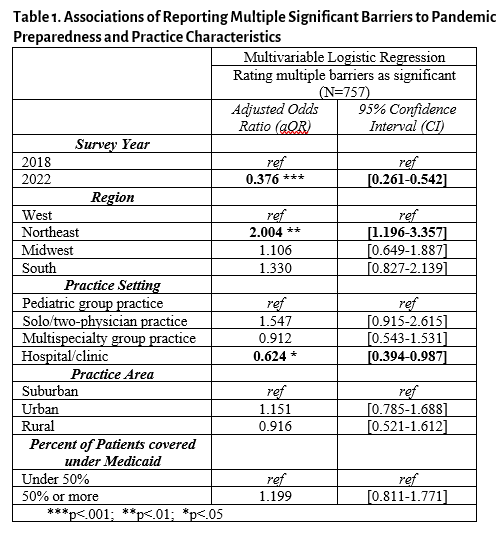
Results: For 4 of the 5 barriers to pandemic preparedness measured (time required, financial cost, lack of knowledge, and lack of administrative buy-in), in 2022 primary care pediatricians were less likely than those in 2018 to rate the factor as a significant barrier to being prepared for a pandemic. At both times, the largest barriers were time required and personnel resources [Figure]. In 2022, 16.9% of pediatricians and 35.2% of those in 2018 reported multiple significant barriers to pandemic preparedness. Adjusting for practice characteristics, compared to 2018, pediatricians in 2022 had lower odds of rating multiple barriers as being significant (p < 0.001) [Table]. Those practicing in the Northeast had about twice the odds of reporting multiple significant barriers as did those in the West (p < 0.01).
Conclusion(s): Primary care pediatricians who experienced the COVID-19 pandemic reported fewer significant barriers to pandemic preparedness than those years earlier who had not experienced such an event. The barriers likely to be of greatest concern were similar from both perspectives.