Hospital Medicine
Session: Hospital Medicine 3
335 - Efficient Rounds: Identifying the Barriers on Pediatric Hospitalist Family-Centered Rounds
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 335
Publication Number: 335.481
Publication Number: 335.481

Lisa J. Fox, DO
Division Chief, Hosptial Medicine
Phoenix Children's
Phoenix, Arizona, United States
Presenting Author(s)
Background: Pediatric hospitalists are responsible for managing patient rounds while balancing learner education and efficiency of rounds. Due to increasing patient complexity, high patient volumes, and other demands, this is challenging yet crucial for throughput, timely patient evaluation, and patient, family, and learner satisfaction. Pediatric hospitalist strategies for effective rounds management are difficult to assess as rounds are typically conducted independently. Peer observation can be used to evaluate rounds and identify barriers to timeliness.
Objective: To utilize peer observation to identify common barriers to rounds efficiency for pediatric hospitalists on family-centered rounds.
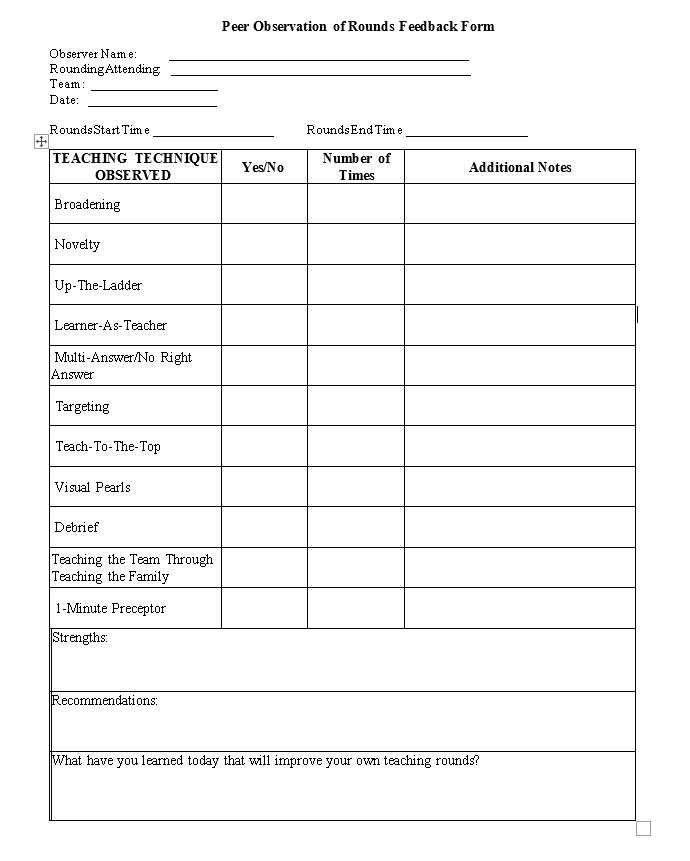
Design/Methods: This observational study was conducted at a tertiary care pediatric hospital between July 2022 - July 2023. All pediatric hospitalists were eligible to participate. The program was voluntary and incentivized. Participants attended a pre-session to orient them to a rounds observation guide (Figure 1). Typical census per rounds session was 14-15 patients. Three separate rounds sessions were observed with pediatric hospitalists at different levels of experience (Tiers (T)1, < 6 years post-training; T2, 6-11 years; and T3, >11 years). A post-rounds debrief followed. The total duration of rounds, and barriers to timely rounds (defined as being completed by 11am with a goal duration of
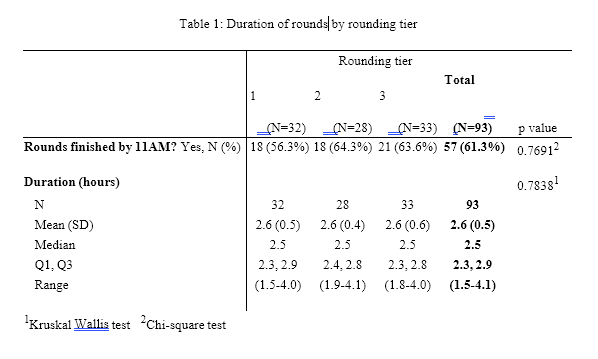
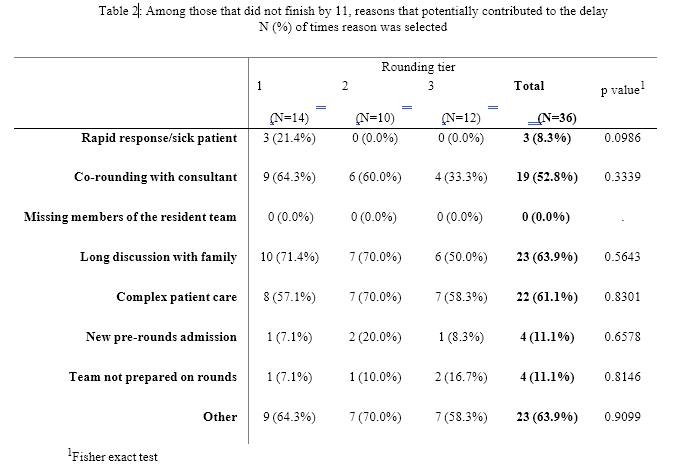
Results: 31 of 48 eligible participants completed the program. 93 observations occurred with 32 in T1, 28 in T2 and 33 in T3. 61.3% of rounds finished on time with a mean duration of rounds of 2.6 hours (Table 1). Observers reported the hospitalist efficiently paced rounds 88.8% of the time. The most common barriers to finishing rounds on time were lengthy discussions with family (63.9%), complex patient care (61.1%), and other (63.9%) (Table 2). The most common barriers cited in the “other” category included the need for interpreters in discussions with families and delayed start to rounds due to morning resident lectures.
Conclusion(s): There are numerous barriers to completing rounds on time, with the need for lengthy discussions and provision of complex care being common sources of delay. Overall, pediatric hospitalists at our institution do an effective job mitigating these barriers and balancing resident education while maintaining efficiency. Further study is needed to determine how existing barriers can be addressed.