Hospital Medicine
Session: Hospital Medicine 5
159 - Variation in the Management of Test Results after Discharge: A Pediatric Hospital Medicine Safety Concern
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 159
Publication Number: 159.1216
Publication Number: 159.1216

Rhiya Dave, DO (she/her/hers)
Resident Physician
Inova Children's Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Failure and delay to follow-up of test results pending at discharge (TRPAD) is a major patient safety concern. Variable handoff practices during transitions of care place further emphasis on this issue. Clinical management of test results has been a focus in adult literature, but few studies exist in the pediatric context.
Objective: The goal of our study is to explore pediatric physicians’ practices and perceptions of the management of TRPAD.
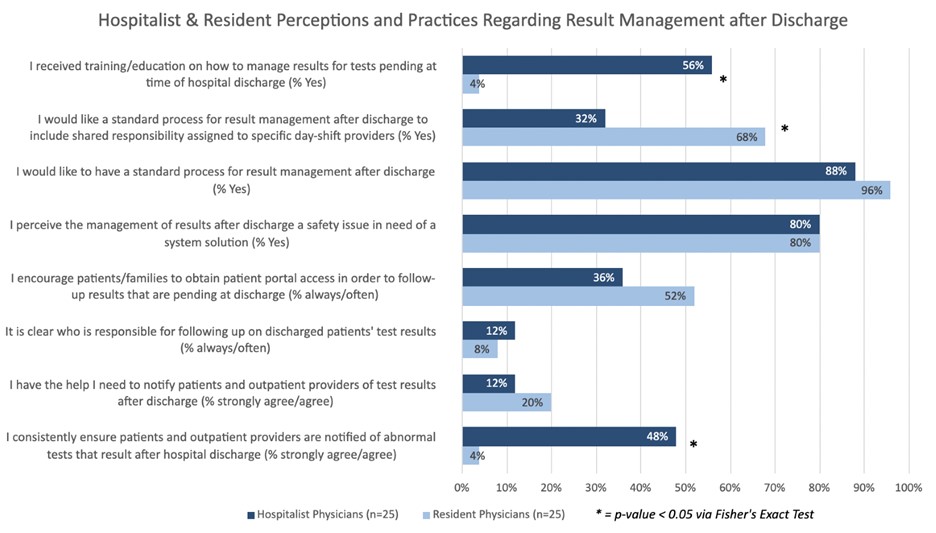
Design/Methods: A primary survey for the pediatric hospitalist was modified from a previously published national survey on primary care practitioners' views on test result management, along with the creation of new questions. Resident physicians completed a selected set of questions extracted from the primary survey. Data were analyzed using Fisher Exact Tests.
Results: Surveys were completed by 25 (89%) pediatric hospitalists and 25 (68%) pediatric resident physicians. 44% (n=11) of hospitalists reported missing results in the past year, while another 44% (n=11) were unsure. Despite this, only 8% (n=2) agree that the missed result led to delay in patient care, while 17% (n=4) were neutral and 22% (n=5) disagreed. 76% (n=19) of hospitalists feel they lack adequate assistance to manage TRPAD and 72% (n=18) use manual cognitive reminders to follow-up on results. Pediatric hospitalists were more likely than residents to use cognitive reminders (72% vs 20%, p=0.0005). Those who had missed a result in the past year were more likely to agree that there are too many alerts to easily focus on the most important ones (100% vs 57%, p=0.02). There's uncertainty regarding who is responsible for managing the result in 88% (n=22) of physicians and 92% (n=23) of residents. 80% (n=20) of pediatric hospitalists and 80% (n=20) of residents agreed that result management is a safety issue in need of a system solution. Although 100% (n=25) of pediatric hospitalists and 96% (n=24) of residents agreed to creating a standardized process for results management, residents were more likely to want this to be a shared responsibility (68% vs 32%, p=0.02). 56% (n=14) of pediatric hospitalists reported receiving formal education on result management and 76% (n=19) of residents would like training.
Conclusion(s): Pediatric hospitalists and residents are concerned about the management of TRPAD and considerable variability exists in current practices. Further improvements include development of a formal resident curriculum regarding patient result management and a standardized process for TRPAD management.