Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 4
261 - Successful Implementation of a Resident-Driven Social Determinants of Health Screen to Address Health Needs in a Community Inpatient Pediatric Unit
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 261
Publication Number: 261.1201
Publication Number: 261.1201

Ria Gupta, BS (she/her/hers)
Medical Student
Johns Hopkins University School of Medicine
Katy, Texas, United States
Presenting Author(s)
Background: Social determinants of health (SDoH) widely impact health outcomes, including in the inpatient setting. Screening for SDoH is an important quality measure, but less than 30% of hospitals report formal inpatient screening. As first-line providers, resident physicians are uniquely positioned to address SDoH needs, but it is unclear how effective resident-driven SDoH screening may be.
Objective: We assessed the impact of a resident-driven SDoH screen on frequency of documentation of SDoH needs and referrals.
Design/Methods: In July 2022, an SDoH screening workflow was implemented in the inpatient pediatric unit of Ascension Saint Agnes Hospital, the community site of the Johns Hopkins Pediatric Residency Program. The 6-item screen was integrated into note templates with the option to defer. Residents were instructed on how to complete the screen and respond to positive screens. We performed a retrospective chart review of patients discharged during equivalent time periods pre- (1/1/2022-6/30/2022) and post- (1/1/2023-6/30/2023) implementation; the pre-implementation time period also included a pilot of the screen (5/11-6/30/2022), the data for which was collected for quality improvement but excluded from the current analysis. We abstracted patient characteristics and outcomes from the electronic medical record through a combination of manual chart review (including SDoH outcomes documented in notes) and automated report. Chi-square and Mann-Whitney tests were used to compare cohort data. The study was approved by the Johns Hopkins Medicine & Ascension Institutional Review Boards.
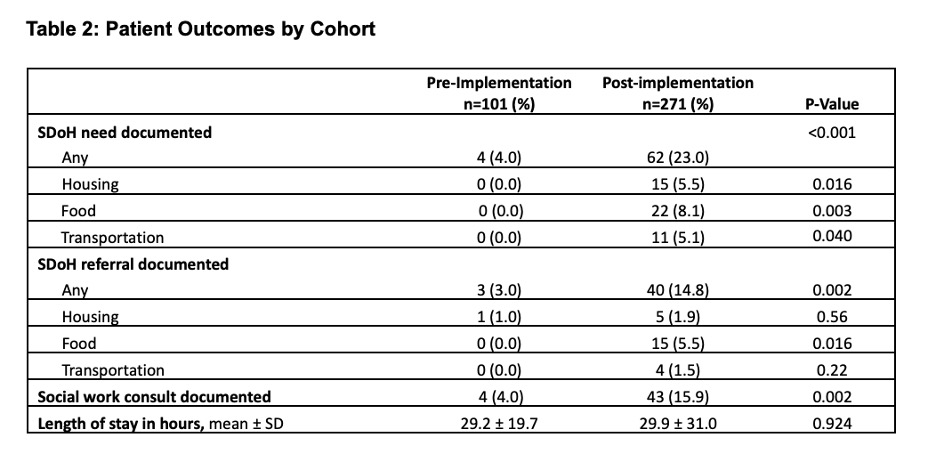
Results: Three hundred seventy-two patients were studied (pre-implementation: 101 patients; post-implementation: 271 patients. 130 (48.0%) patients had completed screens documented post-implementation. There were no significant differences in cohort characteristics (Table 1). Post-implementation, patients were more likely to have SDoH needs documented overall (23.0% vs. 4.0%, p< 0.001) and across housing, food, and transportation domains (Table 2). They also were more likely to have an SDoH referral overall (14.8% vs. 3.0%, p=0.002), for food insecurity (5.5% vs. 0.0%, p=0.016), and to have a SW consult documented (15.9% vs. 4.0%, p=0.002). Length-of-stay was not affected.
Conclusion(s): Patients had significantly increased documentation of SDoH needs and referrals after the implementation of a resident-driven SDoH screen. Future work includes assessment of other patient outcomes, including readmissions, and analysis of resident attitudes surrounding SDoH screening.
.jpg)