Hospital Medicine
Session: Hospital Medicine 3
333 - Creating a Learning Environment on Family Centered Rounds: A Peer Observation of Pediatric Hospitalists
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 333
Publication Number: 333.499
Publication Number: 333.499
.jpg)
Reina Patel, DO (she/her/hers)
Pediatric Hospitalist
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Pediatric hospitalists (PH) are responsible for providing high quality care in the hospital setting while teaching learners and maintaining a learning environment. This skill is rarely taught during medical training. Peer observation is a collaborative tool with potential for mutual benefit; offering the observer an opportunity to learn new strategies and the individual observed objective feedback on the learning environment created.
Objective: Utilize peer observation to evaluate behaviors used by PH that impact the learning environment on clinical rounds.
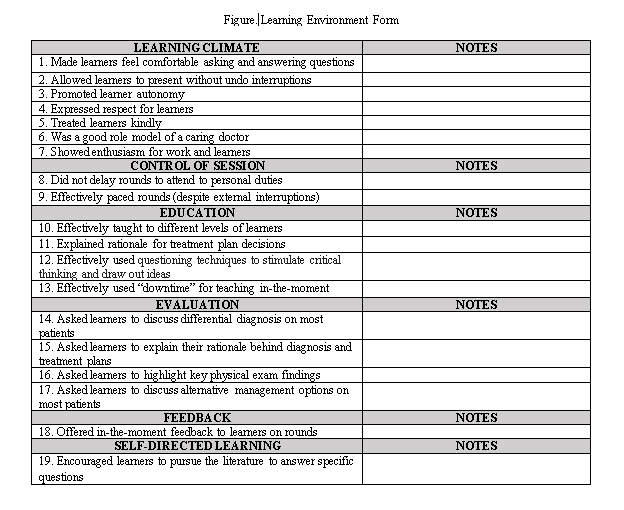
Design/Methods: This prospective observational study was conducted at a tertiary care pediatric hospital between 7/2022-7/2023. All PH division members were eligible to participate. The program was voluntary and incentivized. Participants attended a preliminary session where a Learning Environment survey was reviewed. The 19 target behaviors were divided into 6 categories: Learning Environment, Control of Session, Education, Evaluation, Feedback, and Encouragement of Self-Directed Learning (Figure). Each participant observed three occurrences of rounds with PH at different levels of experience (Tiers (T)1, < 6 years post-training; T2, 6-11 years; and T3, >11 years). A post-rounds debrief followed. Forms were collected and analyzed utilizing the Chi Square test.
Results: 31 of 48 eligible participants completed the program. Of the total 93 observations, documentation was incomplete on 13. The 19 target behaviors were assessed in the remaining 80 observations, with only 1 behavior observed less than 75% of the time, and the remainder ranging from 77.9 - 100% (Table). 6 out of 7 behaviors under Learning Climate were utilized most frequently (100%). The least observed behaviors were “encouraged learners to pursue the literature to answer specific questions” (63.3%), “offered in-the-moment feedback to learners on rounds” (77.9%), and “asked learners to discuss differential diagnosis in most patients” (78.2%) (Table). The only behavior with a significant difference noted between tiers of experience was “asked learners to highlight key physical exam findings” (T1 86.2%; T2 65.2%; T3 92.6%; p value = 0.03).
Conclusion(s): Our study demonstrates that pediatric hospitalists at our institution utilize a variety of behaviors to create a professional learning environment and provide resident education. Little difference was seen between hospitalists at different levels of experience. Future directions include augmentation of PH education to utilize the least observed behaviors and correlation with learner perceptions of learning environment on PH rounds.
.jpg)
