Hospital Medicine
Session: Hospital Medicine 4
134 - Discharge antimicrobial stewardship for common pediatric infections
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 134
Publication Number: 134.1193
Publication Number: 134.1193

Jayme Wilder, MD (she/her/hers)
Hospitalist
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
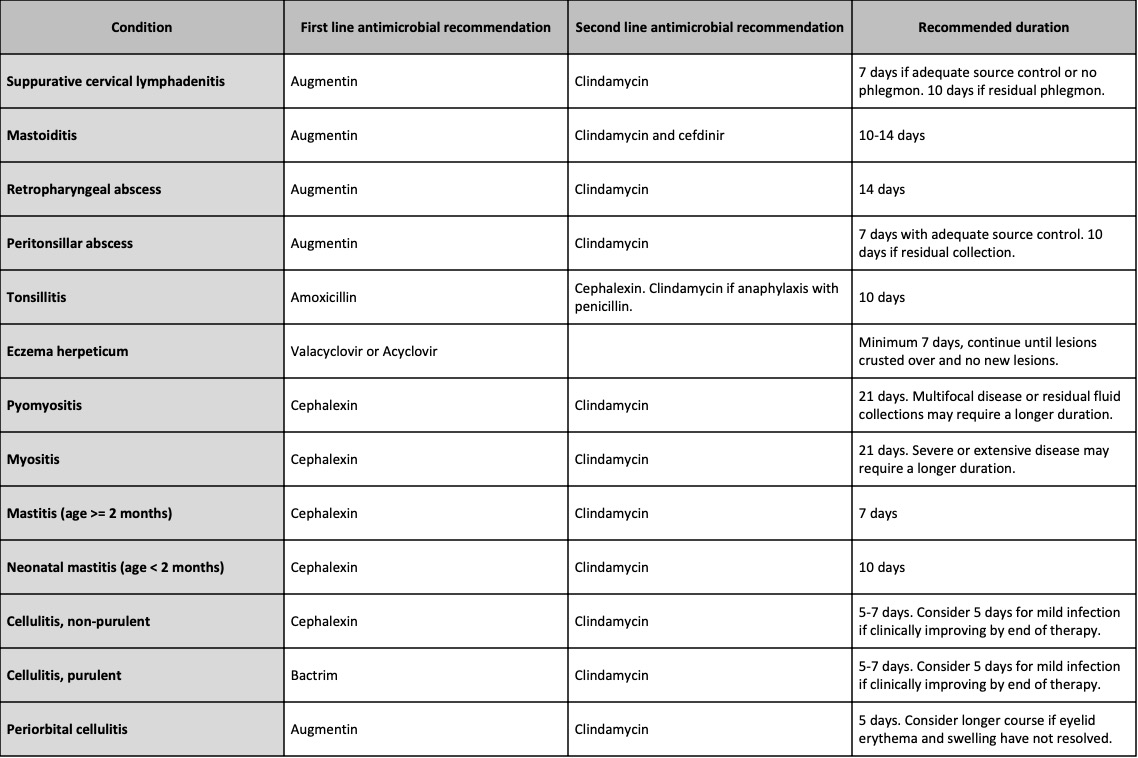
Background: Judicious antibiotic use is critical to prevent resistance and avoid adverse effects of unnecessary use. Antimicrobial stewardship (AS) optimizes antibiotic prescribing and thus patient safety and outcomes, but efforts have focused on inpatient settings. Recognizing AS at care transitions may further improve antibiotic use, we promoted appropriate antibiotic selection and duration at time of discharge for patients admitted to the Pediatric Hospital Medicine (PHM) service with common pediatric head/neck and skin/soft tissue infections (Table 1) using a quality improvement (QI) framework.
Objective: For patients admitted to PHM with a primary diagnosis in Table 1, we aimed to increase the percentage discharged with an appropriate antibiotic and duration (from 71% to 90% and 52% to 75%, respectively) within 12 months.
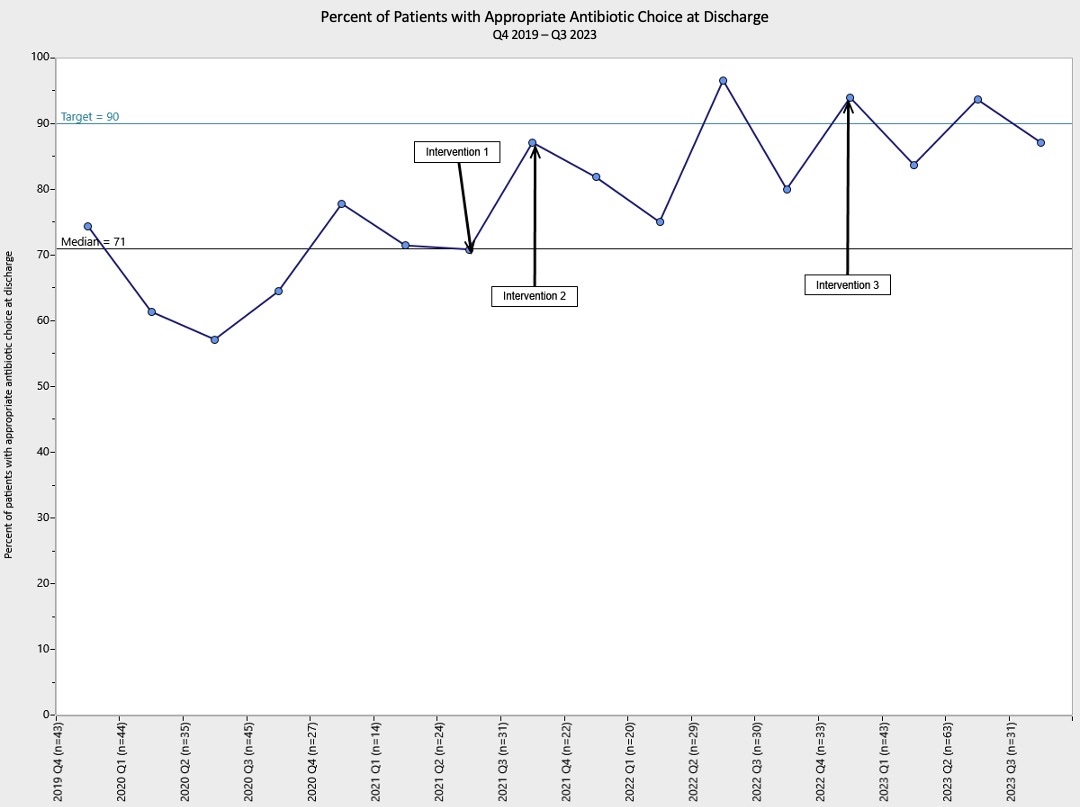
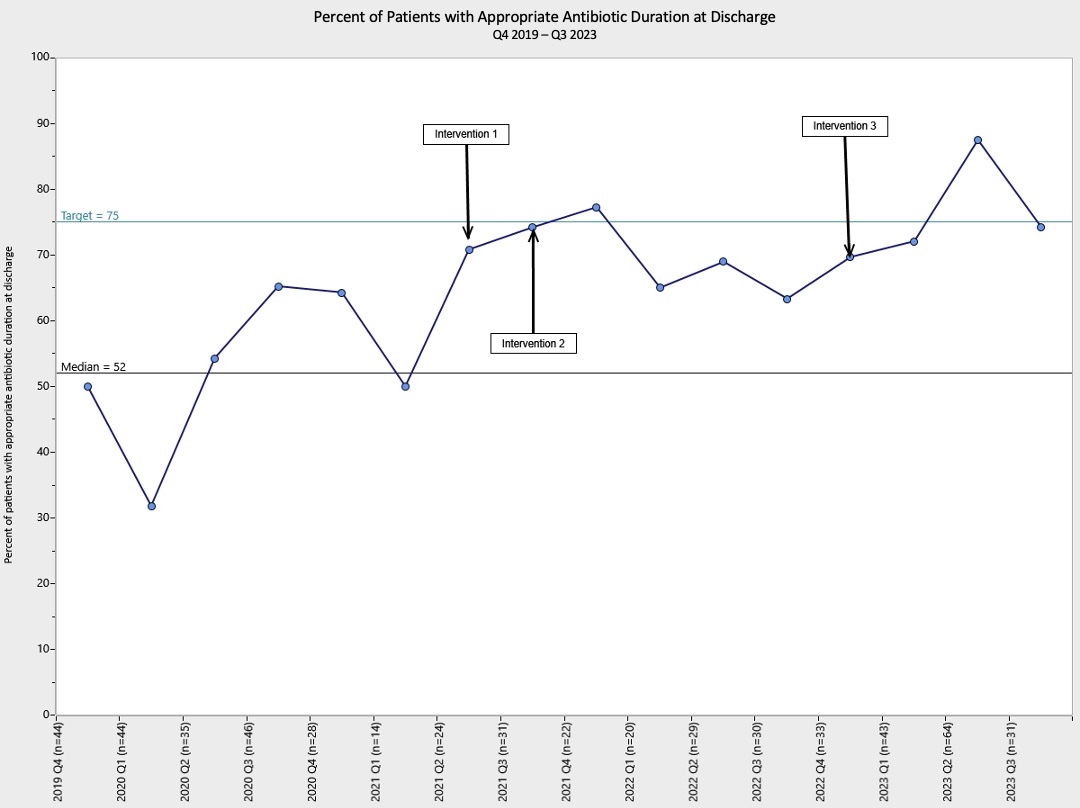
Design/Methods: Representatives of AS, Infectious Diseases, PHM, and Otolaryngology at our quaternary children’s hospital formulated evidence-based recommendations for empiric enteral antibiotic selection and total (intravenous plus enteral) duration (Table 1). Using the Institute for Healthcare Improvement’s Model for Improvement framework, we began Plan-Do-Study-Act cycles in 4/2021, including 1) publishing recommendations in a local web-based AS tool offering guidance on antibiotic selection, dosing, and duration, 2) providing trainee and faculty education at clinical and QI conferences, and 3) creating marketing materials publicizing the antibiogram. We analyzed baseline data (10/2019-3/2021), performed quarterly chart reviews, and tracked practice changes via run charts. Due to small samples of individual infections covered, we assessed measures for conditions collectively. Balancing measures were 14-day Emergency Department (ED) revisits and readmissions.
Results: Since our intervention, the percentage of patients discharged on appropriate antibiotics remained above the baseline median of 71% and is now above our goal of 90% (Fig. 1). The percentage discharged with an appropriate antibiotic duration improved from a baseline median of 52%, to near our goal of 75% (Fig. 2). No change was noted in ED visits or readmissions.
Conclusion(s): Evidence-based guidance on discharge antibiotic selection and duration for common pediatric infections led to improved antibiotic use. Given the success of this initiative, we have begun applying the methodology to additional infections, including community-acquired pneumonia, Lyme meningitis and arthritis. This QI initiative demonstrates the potential benefits of AS during care transitions.