Hospital Medicine
Session: Hospital Medicine 5
150 - Differences in chest radiography rates for bronchiolitis and asthma by race, ethnicity, and Social Vulnerability Index
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 150
Publication Number: 150.1195
Publication Number: 150.1195
- SH
Samantha A. House, DO, MPH (she/her/hers)
Associate Professor
Dartmouth Health Children's
Lebanon, New Hampshire, United States
Presenting Author(s)
Background: Chest radiography (CXR) remains common among bronchiolitis and asthma encounters despite its low value in many clinical scenarios. Evolving literature suggests potential racial, ethnic, and socioeconomic disparities in pediatric low-value care, though these patterns are not yet well-characterized.
Objective: We aimed to measure differences in rates of CXR for bronchiolitis and asthma in the emergency department (ED) and inpatient setting by race, ethnicity, and social vulnerability.
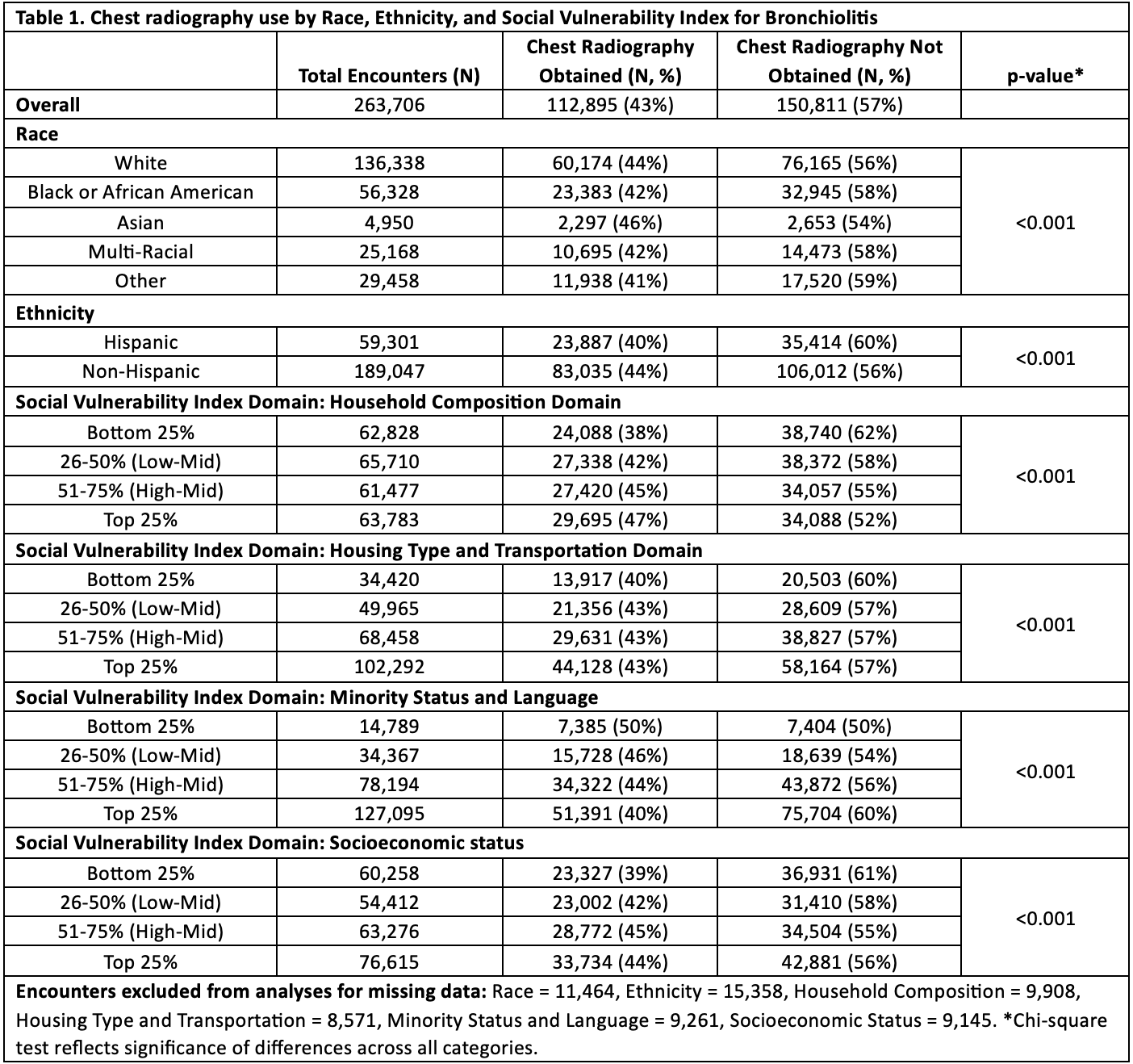
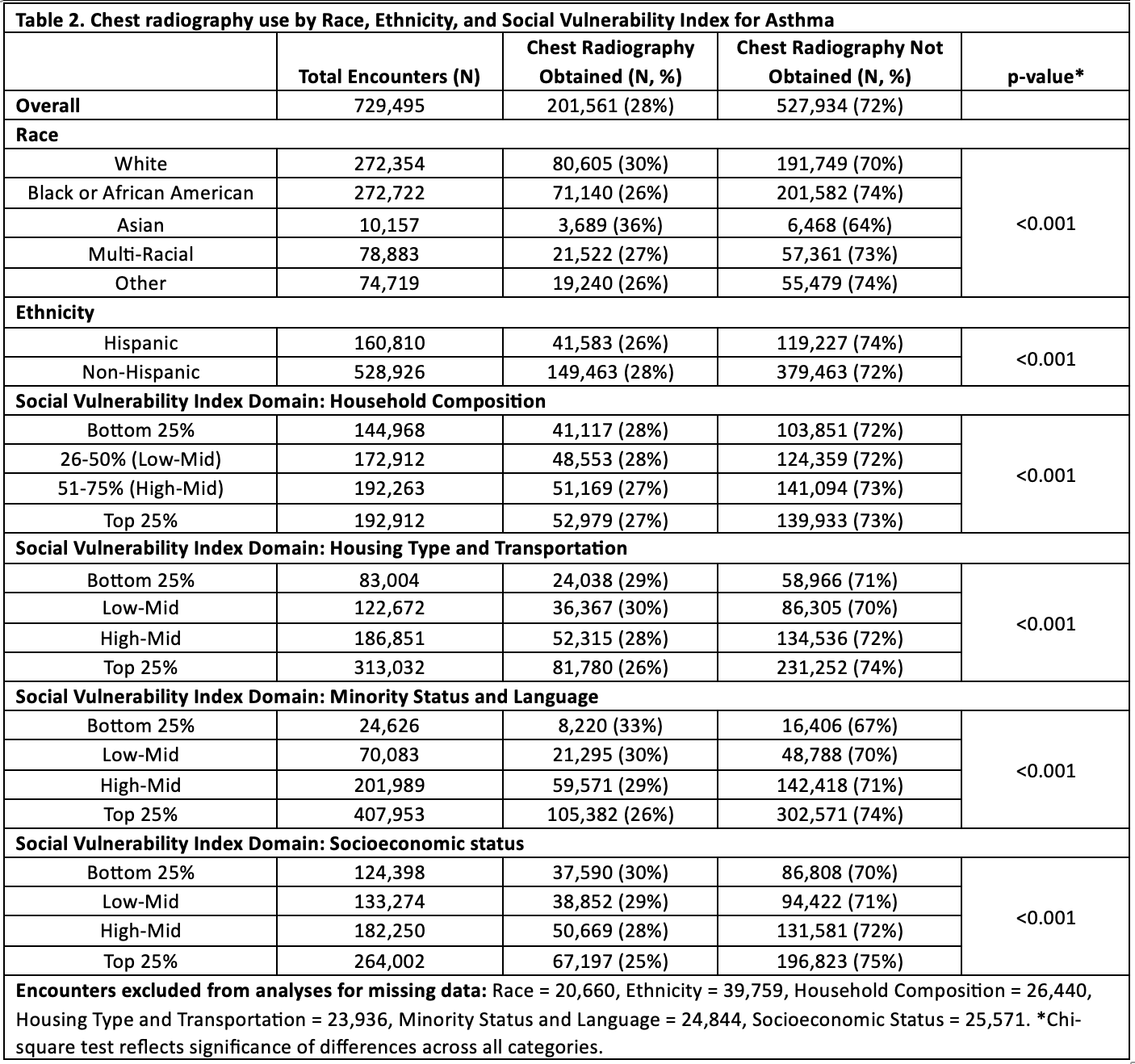
Design/Methods: We conducted a retrospective cohort study of encounters from 7/1/2021 to 6/30/2023 using Epic Cosmos. Cosmos aggregates electronic health record data and represents >9 billion encounters across diverse hospital types. We identified ED visits and hospitalizations for children ages 2-24 months with a diagnostic code for bronchiolitis and ages 3-17 years with a diagnostic code for asthma, excluding outside transfers. We measured differences in CXR rates by race, ethnicity, and the four domains of the Social Vulnerability Index (SVI): Household Composition, Housing Type and Transportation, Minority Status and Language, and Socioeconomic Status. The SVI is a measure of relative neighborhood vulnerability; higher quartiles indicate greater vulnerability. Encounters with missing data were excluded from variable-specific analyses. Differences in CXR rates by predictor variables were measured using chi-square tests.
Results: Overall, CXRs were obtained in 43% of 263,706 eligible bronchiolitis encounters (Table 1) and 28% of 729,495 eligible asthma encounters (Table 2). In both conditions, CXR was most common among children of Asian race, followed by children of White race; children identifying as Black, Multi-racial, or other races were less likely to receive CXR (p < 0.001). By ethnicity, CXR rates were higher among non-Hispanic than Hispanic children for both conditions (p < 0.001) (Tables 1 and 2). For bronchiolitis, increases in CXR rates were observed as SVI increased for 3 domains; the exception was the Minority Status and Language domain, in which CXR rates decreased as SVI increased (Table 1). For asthma, CXR rates were lowest among children in the most vulnerable quartiles for all SVI domains (Table 2).
Conclusion(s): Similar racial and ethnic differences in CXR rates were observed in bronchiolitis and asthma, with the highest rates observed among Asian and White children and those identifying as non-Hispanic. CXR patterns by SVI differed by condition. These findings should be considered when assessing approach to and implications of deimplementation efforts for these services.