Cardiology
Session: Cardiology 2
157 - Leveraging Real World Evidence Based Machine Learning to Enhance Pediatric Cardiovascular Clinical Practice and Research in Pediatric Congenial Heart Disease (2012-2023)
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 157
Publication Number: 157.2872
Publication Number: 157.2872
- GA
Gianni Amato, JD, MPH, MBA
TriNetX
New York, New York, United States
Presenting Author(s)
Background: Congenital cardiovascular defects (CCD) pose a significant public health concern among pediatric patients in the United States. Approximately 12.3 per 1000 children in the US are affected, equating to about 40,000 infants born with congenital heart defects annually. Around 25% require invasive interventions within the first year of life. In 2017, CCDs affected 466,566 individuals with 60% under the age of 20. CCD-related mortality is a leading cause of infant mortality from birth defects at 21.6%.
Objective: We conducted a comprehensive 2012-2023 EHR data analysis of 60,989 pediatric patients diagnosed with CCD, utilizing the TriNetX US Dataworks, database and convolutional and recurrent neural networks to predict clinical outcomes, including hospitalizations and mortality.
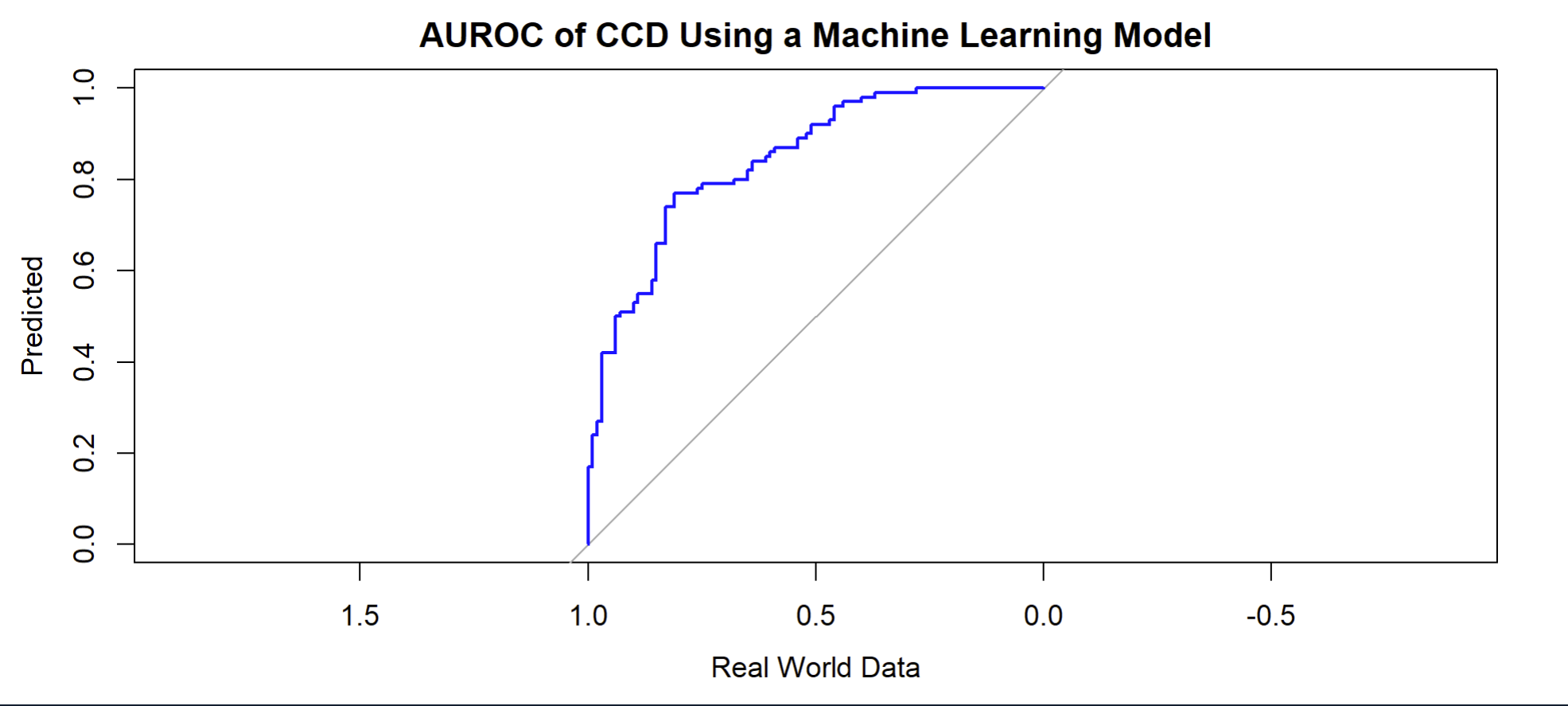
Design/Methods: We conducted a comprehensive 2012-2023 EHR data analysis of 60,989 pediatric patients diagnosed with CCD, utilizing the TriNetX convolutional and recurrent neural networks to predict clinical outcomes, including hospitalizations and mortality. We used advanced machine learning techniques to predict outcomes in pediatric CCD using real world data. Descriptive statistics were used to characterize demographics and and clinical characteristics of the cohort while frequentist methods were used to create results for accuracy, precision, recall, F1 score, AUROC and AUPRC.
Results: Our diverse patient cohort, predominantly with a mean age of 9 and a 54% male predominance, included 60% individuals of European descent, 14% of African descent, 3% of Asian descent, and 15% with unknown racial backgrounds. Pediatric patients of African descent diagnosed with CCD experienced significantly higher hospitalization and mortality rates. The model demonstrated an AUROC of 0.95, with a 92% success rate, 89% precision, and 87% recall.
Conclusion(s): Advanced machine learning techniques offer potential for predictive analytics in pediatric CCD. Our findings spotlight the importance of diverse patient stratification and the value of EHR data in enhancing pediatric cardiovascular research. The model's remarkable accuracy, precision, recall, F1 score, and exceptional AUROC and AUPRC values collectively attest to its proficiency in predicting hospitalizations and mortality. This predictive capability heralds a transition toward anticipatory care in pediatric cardiology, providing valuable insights for clinical professionals. These insights empower them to enhance tailored treatment approaches and optimize the allocation of healthcare resources for CCD, ultimately improving patient care and outcomes.