Sedation Medicine
Session: Sedation Medicine
81 - Increase Referrals for Use of Sedation for Children Undergoing Procedures in the Acute Care Setting
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 81
Publication Number: 81.1174
Publication Number: 81.1174

Sunniya Basravi, DO (she/her/hers)
Clinical Assistant Professor
Stanford University School of Medicine
Redwood City, California, United States
Presenting Author(s)
Background: There have been trends of performing painful procedures at the bedside without time to fully prepare the patient, sometimes requiring patients to be held down to complete procedures that can be painful without proper support. Concurrently pediatric hospitalist provided sedation programs have increased significantly in the last decade and there is an increasing recognition in the role that sedation plays in reducing medical trauma. At our children’s hospital, we have an established hospitalist sedation program. However, sedation was being underutilized in the acute care setting for medical procedures leading to suboptimal patient, family, provider, and staff experiences and contributing to increased stress, procedural anxiety and emotional trauma.
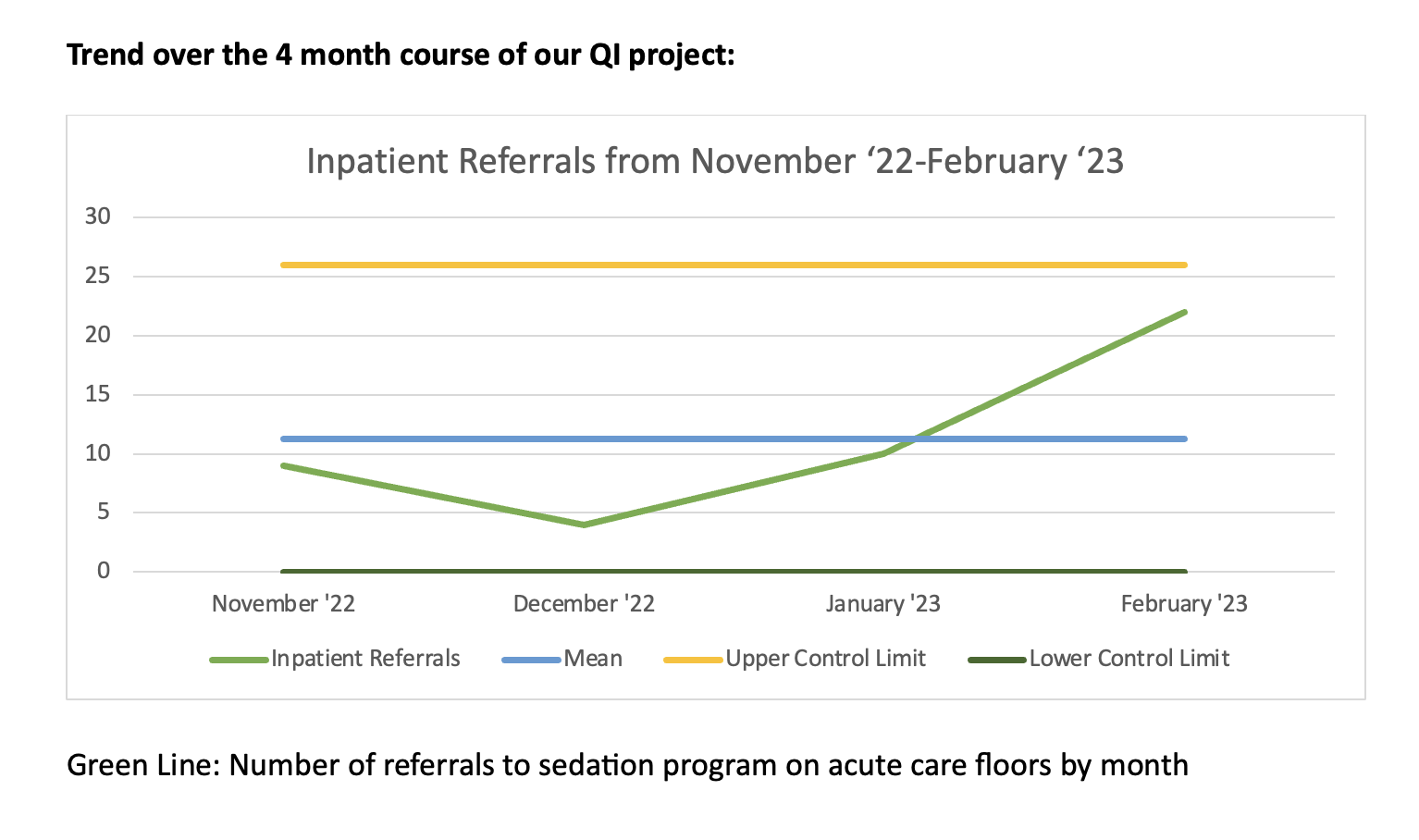
Objective: We aimed to improve our current processes and referrals to help increase utilization of sedation for procedural support in order to help patients better cope with difficult procedures. Our goal was to increase referrals to the sedation program on the acute care floors from a mean of 7 to 10 per month within the next 4 months.
Design/Methods: We approached this problem using the A3 method for quality improvement (QI). We conducted a current state analysis and identified the following 3 key drivers: General knowledge gap about the hospitalist sedation program, lack of standard consult process for sedation, and no standard education about procedural sedation. To target the knowledge gap we used several different platforms to raise awareness of our program including posting on the residency forum, daily reminders to the charge nurse on each unit, and advertising our program on hospital screensavers. We then created tip sheets outlining the consult process and distributed this among multidisciplinary providers. To increase understanding of sedation, we created a mini module on sedation and posted it via QR code on the sedation website, gave multiple didactic lectures, and created educational material that could be shared in parent groups.
Results: Within two months of implementing our interventions we exceeded our goal and continued to see a rise in sedation consults each month with an average of 11.25 sedation referrals on the acute care floors. In particular we saw increased referrals for sedation from general pediatrics and oncology.
Conclusion(s): With our interventions, we directly increased patient access to procedural sedation thus reducing pain and anxiety surrounding procedures. This will reduce the chance of negative long- term effects of emotional medical trauma and promote health equity.