Technology
Session: Technology 1
167 - Implementing the 4-Cut Method for Empanelment Requires 5 Steps (Cuts)
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 167
Publication Number: 167.2148
Publication Number: 167.2148
.jpg)
Paul M. Darden, MD (he/him/his)
Professor
University of Arkansas for Medical Sciences College of Medicine
Little Rock, Arkansas, United States
Presenting Author(s)
Background: Continuity of care is important and associated with improved patient satisfaction, patient outcomes, provider satisfaction and lower costs of care. However, effective empanelment of patients is challenging.
Objective: To implement a methodology, 4-cut method (Wajnberg 2019) in primary care practices and identify gaps.
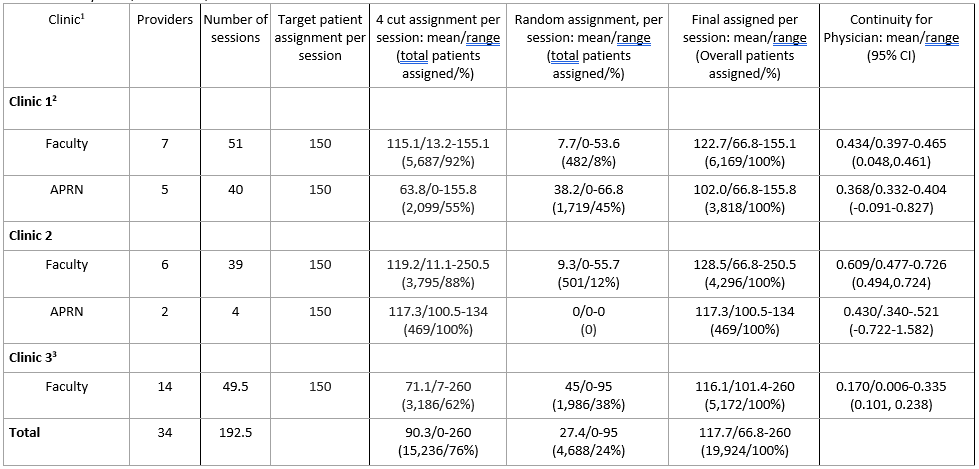
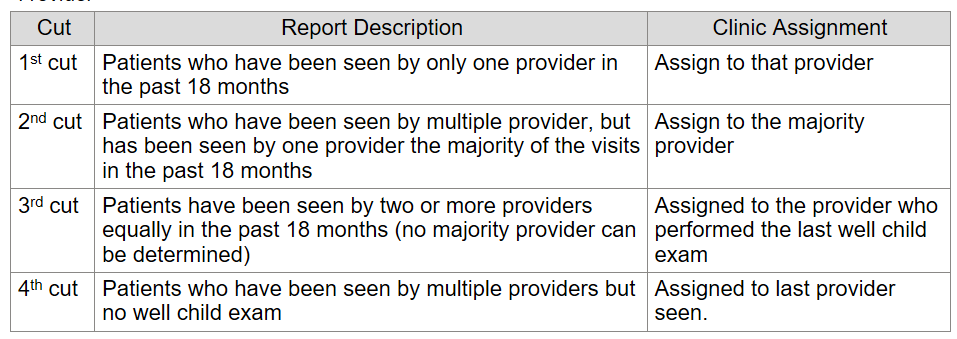
Design/Methods: Eighteen months of visit data for patients < 21 years was pulled from the electronic health record (EHR) to use for assignment. Due to EHR limitations, assignment was external to the EHR. The 4-cut methodology empanels patients to the provider to whom they were most engaged. The 4-cut method sequentially assigns patients, based on engagement with the provider (Table 2). This report covers clinics where patients are not scheduled with trainees or the school-based clinics. Not included in the 4-cut method, patients seen in clinic but not seen by a current provider were randomly assigned. Patients could be seen in any of the clinics based on appointment availability. First, the 4-cut method was done by clinic level to identify their home clinic prior to provider assignment. The target assignment was 150 patients/weekly half-day in clinic. Empanelment was assessed using the Continuity for Physician (Darden 2001) methodology using visits from 7/1/2022-6/30/2023 (academic year 2023) to lessen the effect of provider transitions. For Continuity for Physician calculations, providers who did not see patients in the academic year 2023 were excluded.
Results: Over 18 months, 29,391 unique patients had 85,130 visits to the primary care clinics. There were 10,687 (36.4%) patients seen in more than one clinic. Patients were assigned to clinics using the 4-cut method. Three clinics, 19,924 patients were examined. In cut-1, an mean of 51% of patients were assigned. For cut-2, a mean of 11% of patients were assigned. In cut-3, a mean of 12% were assigned. In cut-4 a mean of 2% of patients were assigned. Overall, the 4-cut method assigned 76% of patients (Table 1), leaving 26% of patients (range; 24%-38%) needing assignment. Examining Continuity for Physician and the 4-cut method, Continuity for Physician is associated with the proportion of patients assigned by the 4-cut method (R2=0.67, P< 0.001) and clinic (R2=0.74, P< 0.001).
Conclusion(s): The 4-cut method is useful for empaneling patients and is supported by the association of Continuity for Physician with clinic and proportion assigned by this method. For most clinics there will need to be a 5th cut for patients who are engaged with the clinic but have never seen a current provider, perhaps random assignment based on panel size.