Newborn Care
Session: Newborn Care
215 - Demographic and Clinical Factors Associated with Sepsis Mortality: An Analysis of National Inpatient Data (2016-2020)
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 215
Publication Number: 215.527
Publication Number: 215.527

ibrahim Qattea, MD (he/him/his)
Fellow
Nassau University Medical Center
East Meadow, New York, United States
Presenting Author(s)
Background: Neonatal Sepsis is a critical public health concern with a substantial impact on healthcare systems and patient outcomes. To address this issue comprehensively, it is crucial to identify the factors contributing to sepsis mortality. This study seeks to investigate the associations between demographic and clinical variables and sepsis-related mortality using a large, de-identified national inpatient dataset.
Objective: The primary objective of this study is to determine the relationships between various demographic and clinical factors and sepsis-related mortality. Specifically, we aim to look for the difference between reporting neonatal sepsis and death due to neonatal sepsis in USA.
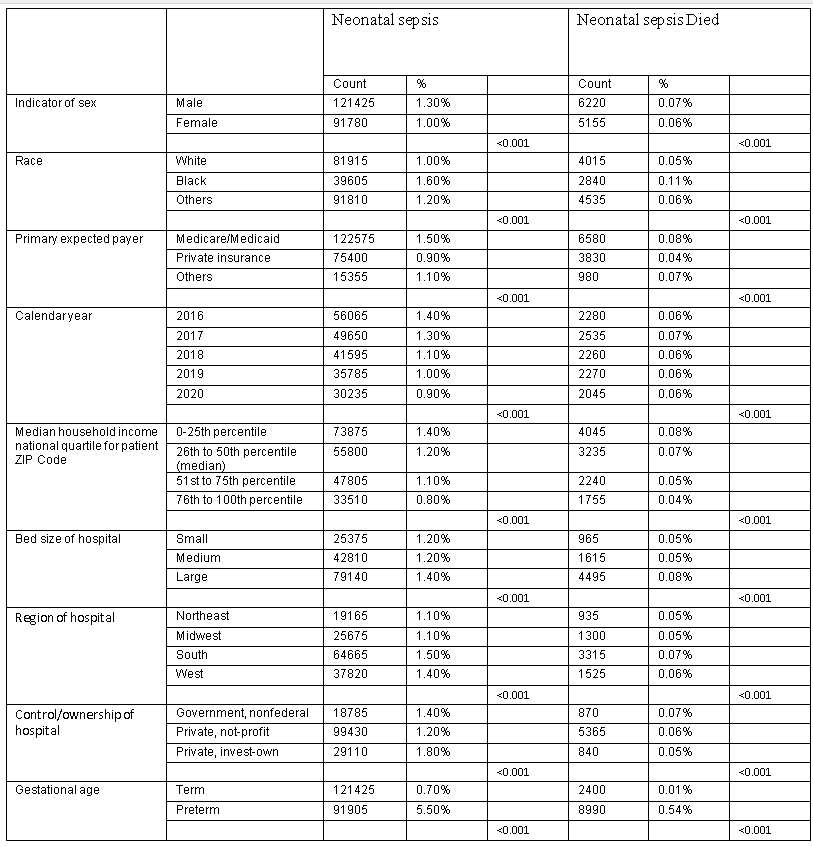
Assess the impact of sex, race, primary expected payer, calendar year, median household income, bed size of hospital, location/teaching status of hospital, region of hospital, and control/ownership of hospital on sepsis mortality rates. Examine the influence of different preterm birth categories and sepsis-related mortality.
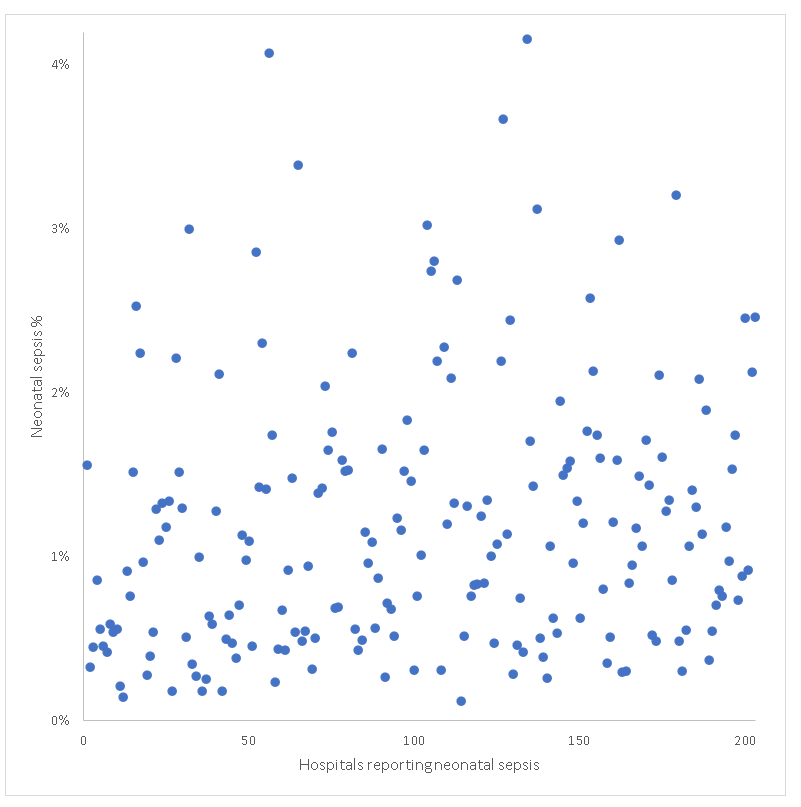
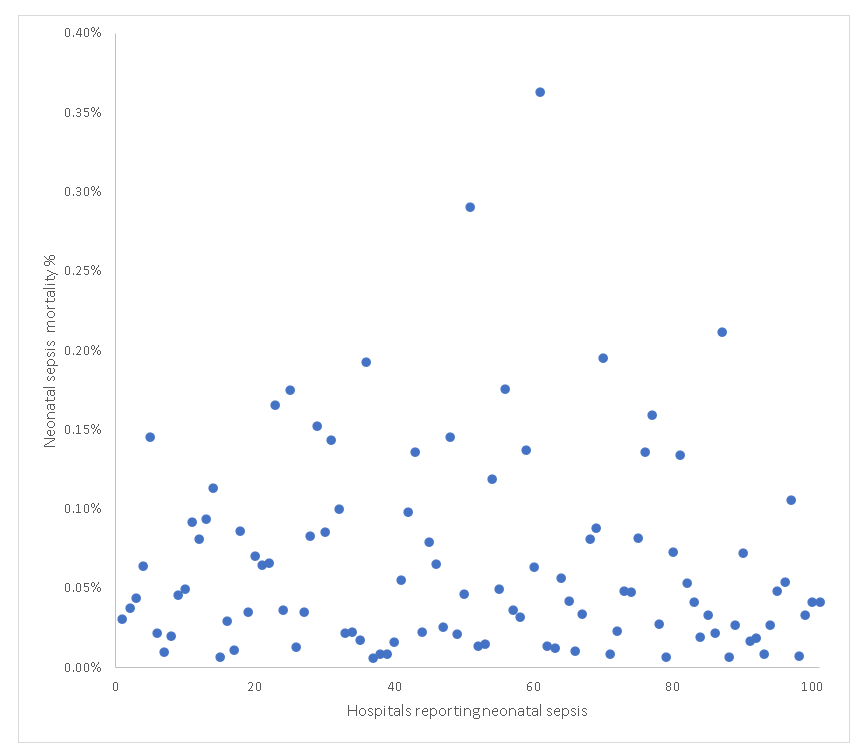
Design/Methods: We utilized the de-identified national inpatient sample dataset from the Healthcare Cost and Utilization Project (HCUP) provided by the Agency for Healthcare Research and Quality (AHRQ) for the years 2016–2020. We looked for the incidence of neonatal sepsis within 203 hospitals in the United States, and we also looked for the neonatal sepsis mortality within 101 hospitals in the United States. We employed appropriate statistical methods, including chi-square tests and logistic regression, to analyze the relationships between the specified variables and sepsis mortality.
Results: There is a big difference in reporting neonatal sepsis (0.21 to 4.2%) and death due to neonatal sepsis (0.01% to 0.36 %)
Our analysis revealed significant associations between various demographic and clinical factors and sepsis-related mortality. Key findings include Sex, race, primary expected payer, and preterm birth categories were strongly associated with sepsis incidence and mortality.
Calendar year, median household income, bed size of hospital, location/teaching status of hospital, region of hospital, and control/ownership of hospital also showed statistically significant relationships with sepsis incidence and mortality.
Conclusion(s): This study provides valuable insights into the hospitals factors contributing to sepsis mortality, highlighting disparities and areas for potential intervention. These findings can inform healthcare policies and practices aimed at reducing sepsis-related deaths and improving patient care outcomes.