Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 1
481 - Identifying implementation strategies for a mobile health tool to guide diagnosis and management of acute pediatric respiratory illnesses in Uganda
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 481
Publication Number: 481.530
Publication Number: 481.530
- LE
Laura E. Ellington, MD, MS (she/her/hers)
Assistant Professor
Seattle Children's
Seattle, Washington, United States
Presenting Author(s)
Background: Acute lower respiratory illnesses (ALRI) are a leading cause of death in young children, with the majority in sub-Saharan Africa. ALRI is a heterogenous group of diseases without a diagnostic gold standard. In resource-constrained settings, case management is challenging, and adherence to case management guidelines is poor. Wheezing illnesses in particular are underdiagnosed and go untreated. We developed the Acute Lower Respiratory Treatment and Evaluation (ALRITE) tool as a point-of-care smartphone-based decision support tool for frontline health workers. ALRITE leverages the World Health Organization Integrated Management of Childhood Illness (IMCI) guidelines, focusing on respiratory care management and wheezing illnesses. We piloted ALRITE in clinical care and identified challenges with health system integration.
Objective: The objective of this study was to identify promising solutions to improve ALRITE implementation using a human-centered, implementation approach.
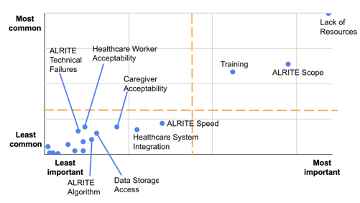
Design/Methods: Mixed methods (QUAL > quant) design with health workers at 8 health centers in the Jinja District, Uganda. We conducted focus group discussions (FGDs) at each site, using the nominal group technique to list all barriers impacting health workers’ ability to care for children with respiratory illnesses and implement ALRITE in clinical care. We then asked health workers to rank barriers by a) importance and b) frequency (how common). We identified the top 5 barriers using go-zone plots and returned to conduct a second FGD per site whereby health workers brainstormed promising solutions to address each barrier, then ranked solutions by a) importance and b) feasibility, using similar techniques to the first FGD.
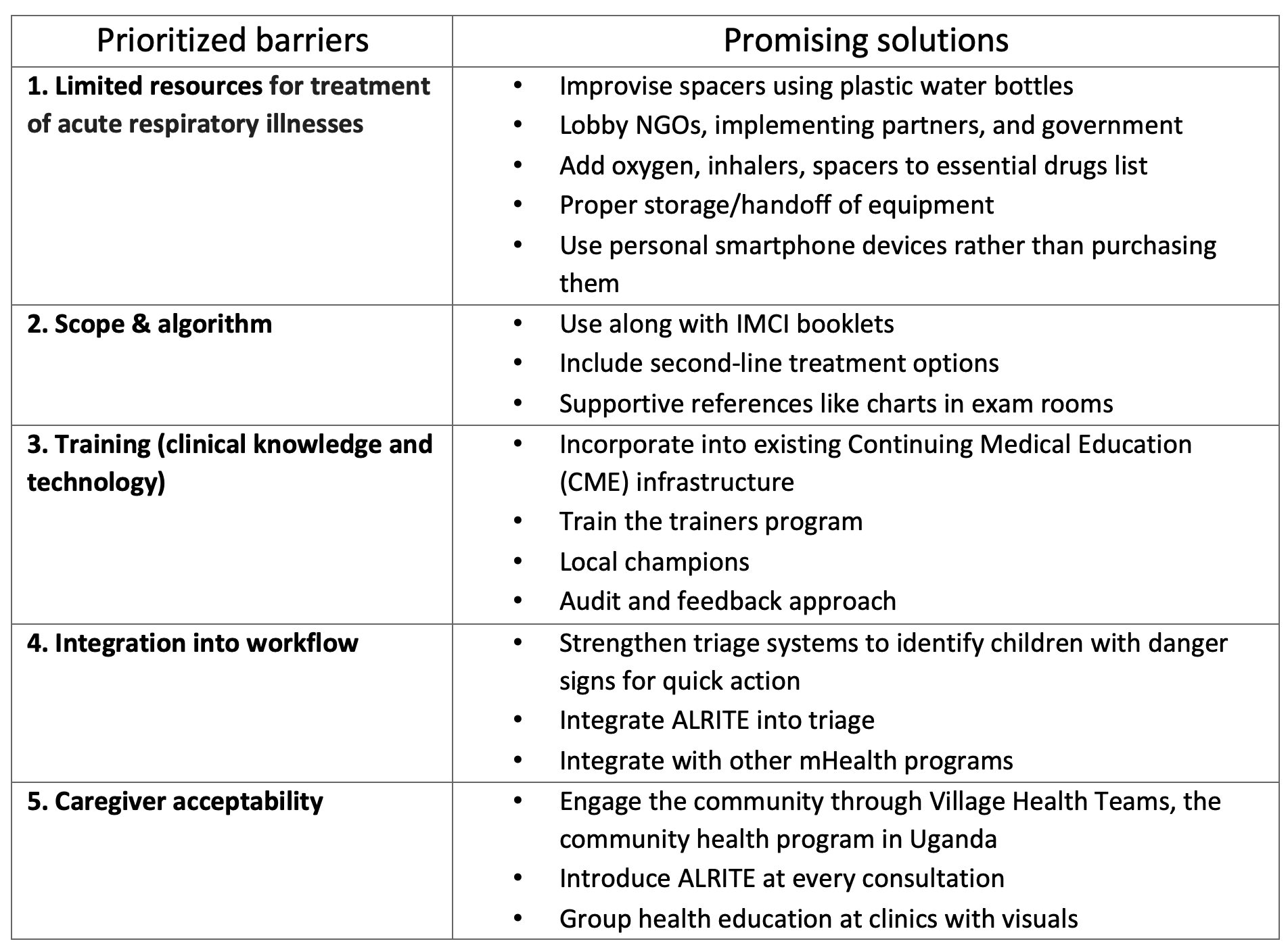
Results: Sixty-six health workers participated from 8 sites. The majority (36%) were registered nurses, 26% were clinical officers, 12% were medical officers, and 26% were technicians or midwives. The top 5 barriers were 1) limited resources for treatment of ALRI, 2) limited ALRITE scope and algorithm, 3) training needs (clinical and technical knowledge), 4) ALRITE integration into workflow, and 5) caregiver acceptability concerns (Figure 1). Examples of linked solutions are found in Table 1.
Conclusion(s): We prioritized addressable barriers to ALRITE use and identified viable solutions. Next steps include ALRITE optimization and evaluation of the refined ALRITE tool in Ugandan health centers.