Medical Education
Session: Medical Education 3
541 - A novel national Women in Neonatology Mentorship Program leads to significant benefits in career development, networking and wellness.
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 541
Publication Number: 541.535
Publication Number: 541.535

Kristen T. Leeman, MD (she/her/hers)
Associate Medical Director, NICU
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: A significant deficiency exists in mentorship of female neonatologists in areas of career development, wellness, and work-life balance. Despite females comprising the majority of the neonatal workforce, disparities in leadership opportunities continue to exist.
Objective: To design a novel national mentorship program for women in neonatology to fill existing gaps and test effectiveness of the intervention.
Design/Methods: Through the American Academy of Pediatrics Women in Neonatology subgroup, we created a 1-year pilot mentorship program using a flipped classroom hybrid format. The 245 participants were placed into mentorship “families” composed of junior, middle career and senior members based upon area of career/ academic interest. “Pre-learning” content for each session was independently reviewed prior to the virtual or in person sessions and the group discussion. Pre and post program surveys assessed mentorship needs, program logistics, effectiveness, and experience.
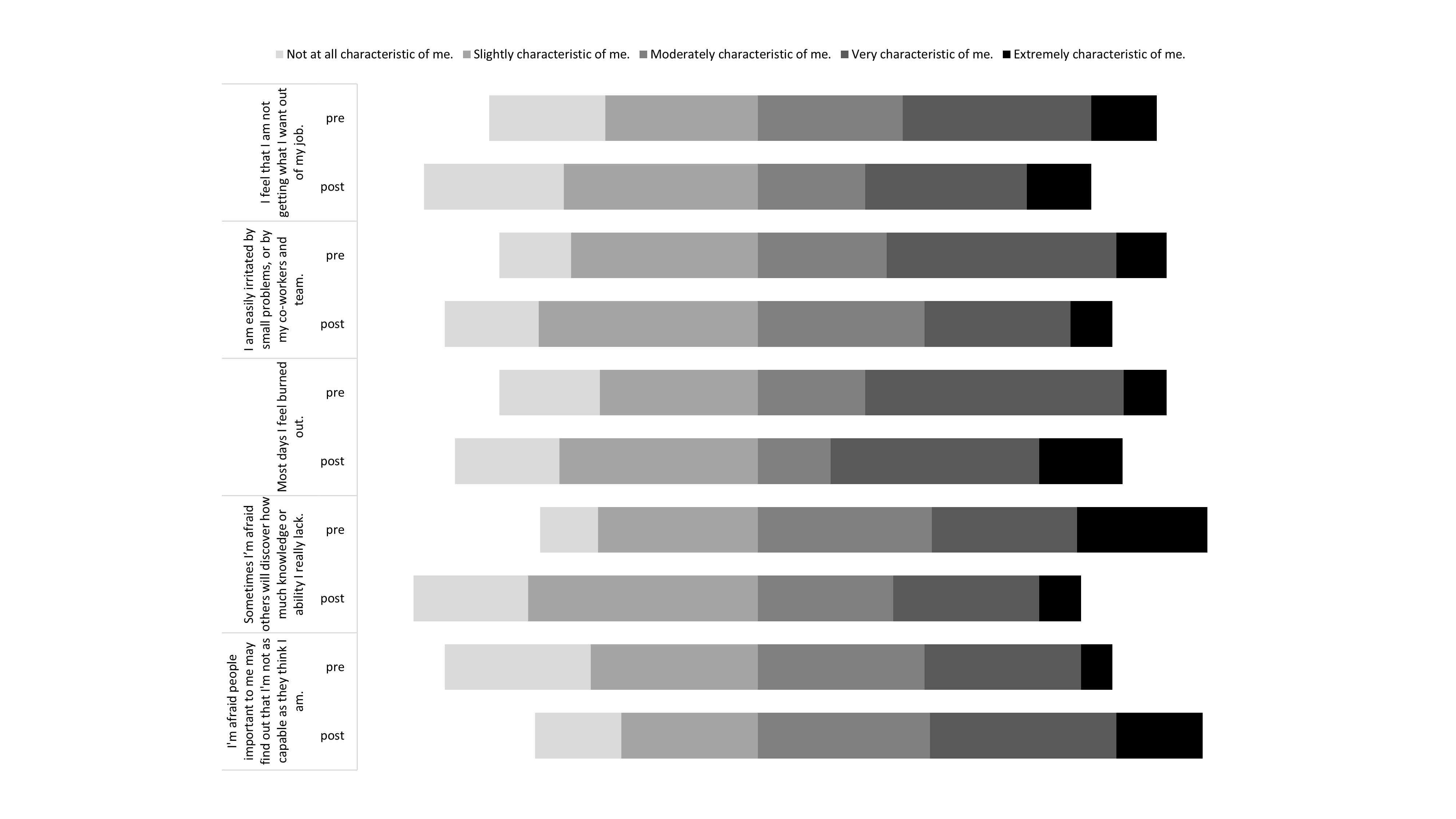
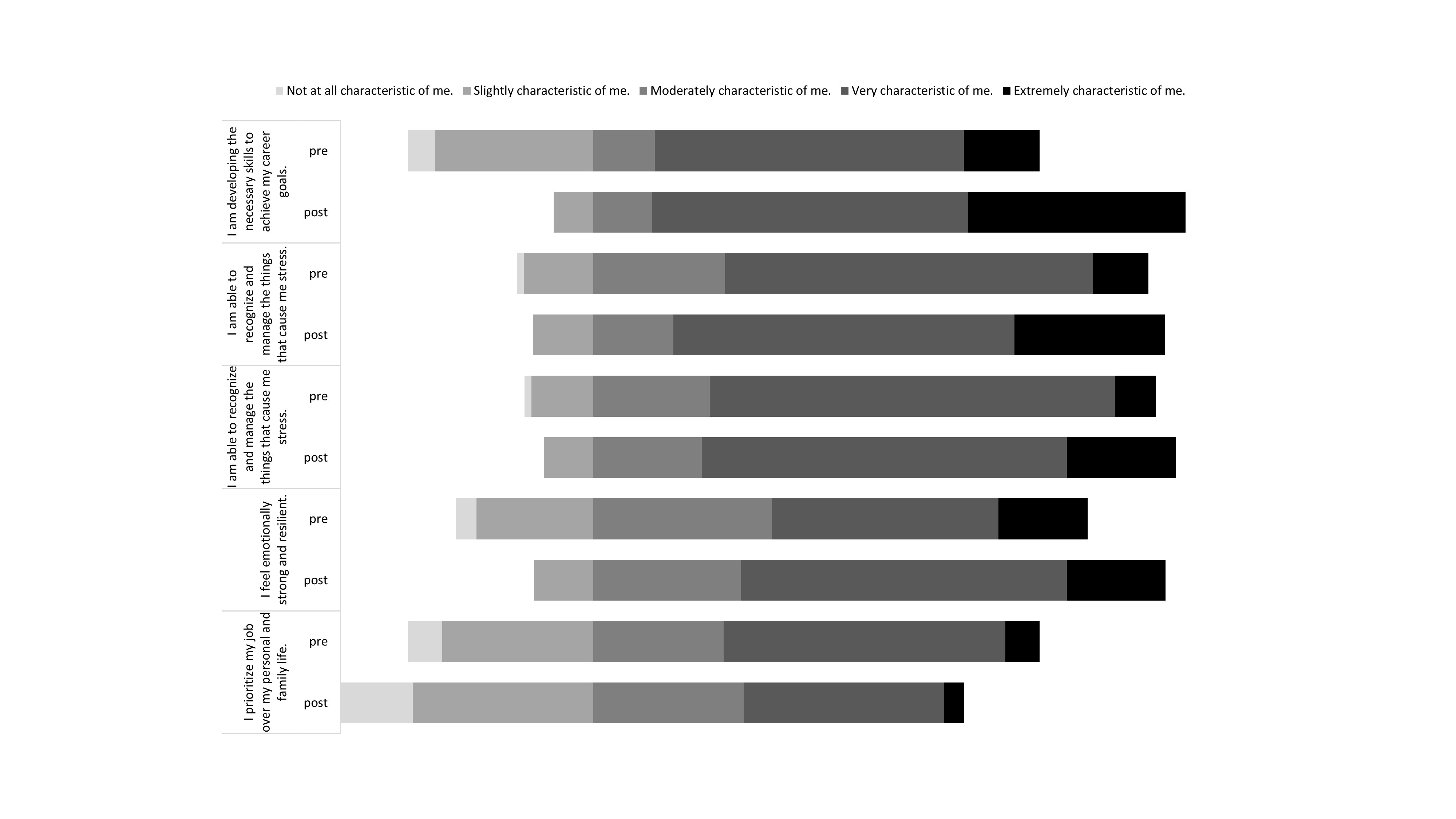
Results: The pre-survey had 93 responses (RR = 38%) and post-survey had 68 responses (RR = 28%). Respondents were from < 7 years of experience (pre 57% vs. post 46%) and > 7 years of experience (pre 43% vs. post 54%). The pre-survey reported inadequate mentorship in work life balance (47%), wellness (46%), and career area (41%). Program participants rated the pre-session content guides as high quality (94%), appropriate length (93%) and highly useful (94%). Importantly, 28% of participants reported that the mentorship program directly led to a career advancement (e.g. speaking opportunity, research collaboration, project involvement). The top mentorship gaps filled by the program were in career advancement (31%), wellness (19%), and work-life balance (22%). Participants reported positive program outcomes as networking/collaborations, sharing of strategies/advice, educational content, and connections/support offered. Nine validated burnout and imposter syndrome questions showed improvement between pre and post scores with an average improvement of 0.39 (sd=0.16) on a 5-point likert scale (Fig 1, 2).
Conclusion(s): A national women in neonatology mentorship program created opportunities for enhanced networks across career levels and geography, and utilized high quality content and group discussions to foster connections. The program directly led to increased career advancement and improved markers of burnout and imposter syndrome in participants. Together, this program created a successful framework to fill mentorship gaps for women in neonatology with possibilities for high generalizability across other medical specialties.