Hospital Medicine
Session: Hospital Medicine 3
331 - Closing Time: Reducing Resident Work Hours on the Pediatric Wards
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 331
Publication Number: 331.536
Publication Number: 331.536

Christopher Vincent, MD (he/him/his)
Resident Physician
Southern Illinois University School of Medicine
Springfield, Illinois, United States
Presenting Author(s)
Background: Excessive work hours and high levels of resident burnout can lead to medical errors, lower quality patient care, and poor academic performance. (1) This is often particularly noted on busy inpatient services such as the pediatric wards. While residency programs monitor duty hours closely per ACGME mandate, a lack of violations can be misleading and is not always reflective of resident workload and wellness. Our residents, particularly interns, were often observed staying after daily sign-out to complete notes and other tasks which prolonged their shift but did not always result in duty hour violations.
Objective: Our objective was to reduce the percentage of weekday occurrences in which any intern on the wards team stayed after the end of their shift in order to complete work from a baseline median of 37% of occurrences to < 20% by May 2023.
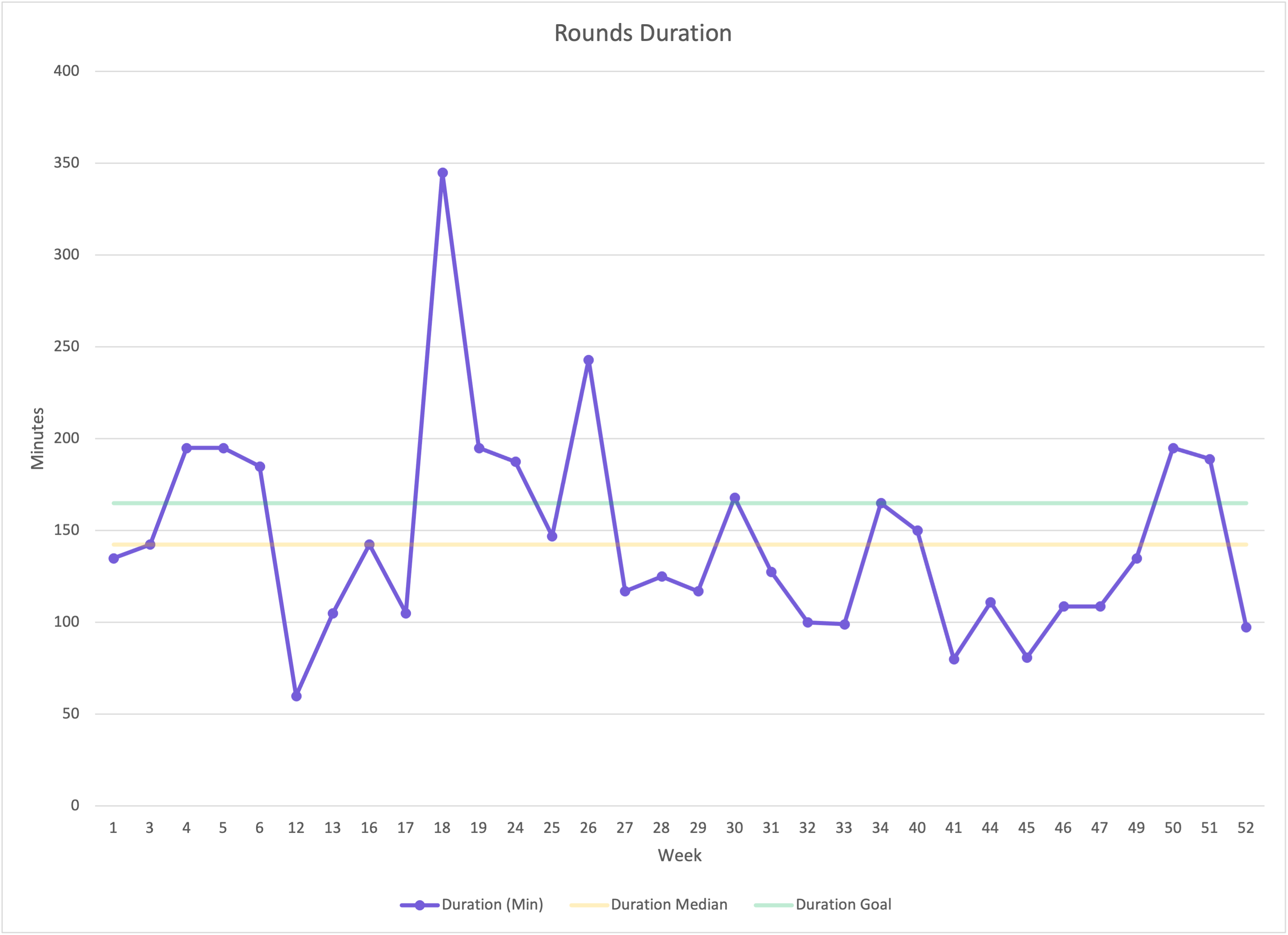
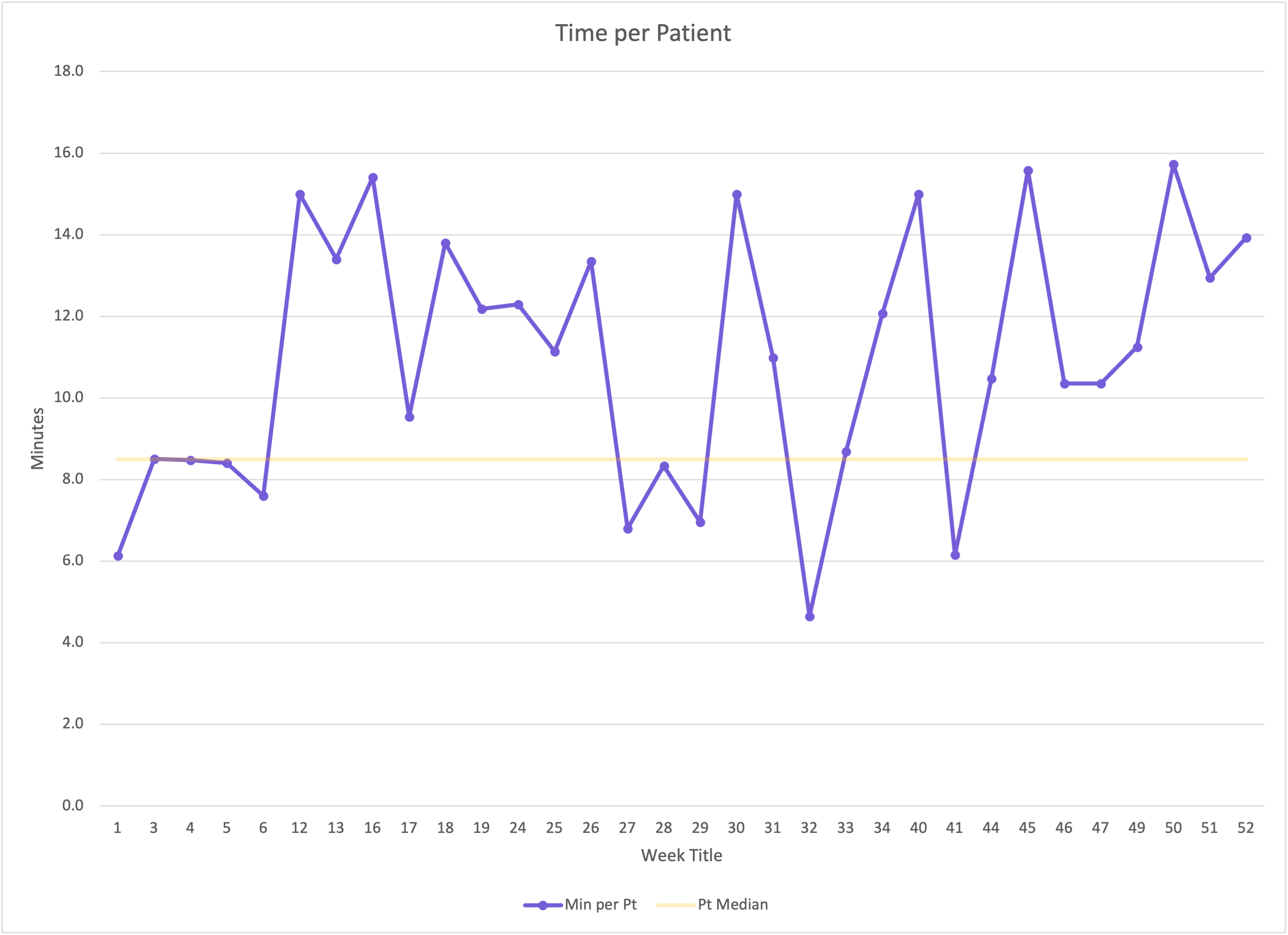
Design/Methods: Data was collected from October 2022 through October 2023, with the primary outcome measure obtained via a paper survey in the team room that any resident could anonymously report how many interns stayed late each day. Process measures included the daily patient census and duration of morning rounds. The balancing measure was average time spent per patient on rounds, to ensure that patient care was not compromised for the sake of efficiency.
Various plan-do-study-act (PDSA) cycles were implemented, with initial interventions focused on reducing the length of morning rounds and redistributing tasks among day and night teams. Later interventions focused on the timing of transitions of care, with PICU to wards transfers being held if occurring within one hour before sign-out and the transition of responsibility for new admissions was lengthened from 30 to 45 minutes before sign-out (i.e. – any admission arriving within 45 minutes prior to sign-out would be the responsibility of the oncoming team). Finally, an off-service moonlighting resident was also introduced to take new admissions if the census reached a certain threshold.
Results: Following the completion of these PDSA cycles, the median occurrences of interns staying after sign-out shifted from 37% to 3% of weekdays, well below our goal of < 20%. The average time spent per patient on morning rounds remained unchanged at approximately 8.5 minutes per patients.
Conclusion(s): These data demonstrate that our interventions were effective in reducing the frequency with which interns stayed late to complete work, without compromising the amount of time spent with patients. Project limitations include variation in patient census and residents’ natural progression of efficiency.
.png)