Neonatology
Session: Neonatal Hematology & Bilirubin Metabolism
459 - Platelet contribution to clot strength in thromboelastometry in preterm septic neonates with thrombocytopenia: Both platelet count and function are considerable
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 459
Publication Number: 459.1157
Publication Number: 459.1157
- GM
Georgios Mitsiakos, MD
Professor
2nd Neonatal Department & NICU, Aristotle University of Thessaloniki, "Papageorgiou" Hospital
Thessaloniki, Thessaloniki, Greece
Presenting Author(s)
Background: Thromboelastometry (ROTEM) is a whole blood, visco-elastic, point-of-care coagulation test that is currently included in many algorithms for the diagnosis and treatment of bleeding. The difference in amplitude between the EXTEM and the FIBTEM ROTEM assays is considered an index of platelet contribution to clot strength (MCFplatelet) guiding management in thrombocytopenic patients. However, recent literature challenges the validity of MCFplatelet suggesting that the difference in maximum clot elasticity (MCEplatelet) is highly accurate.
Objective: We investigated the potential of MCFplatelet and MCEplatelet in reflecting platelet count and function in septic preterm neonates during and their healthy counterparts, simultaneously assessing ROTEM and platelet flow cytometry tests.
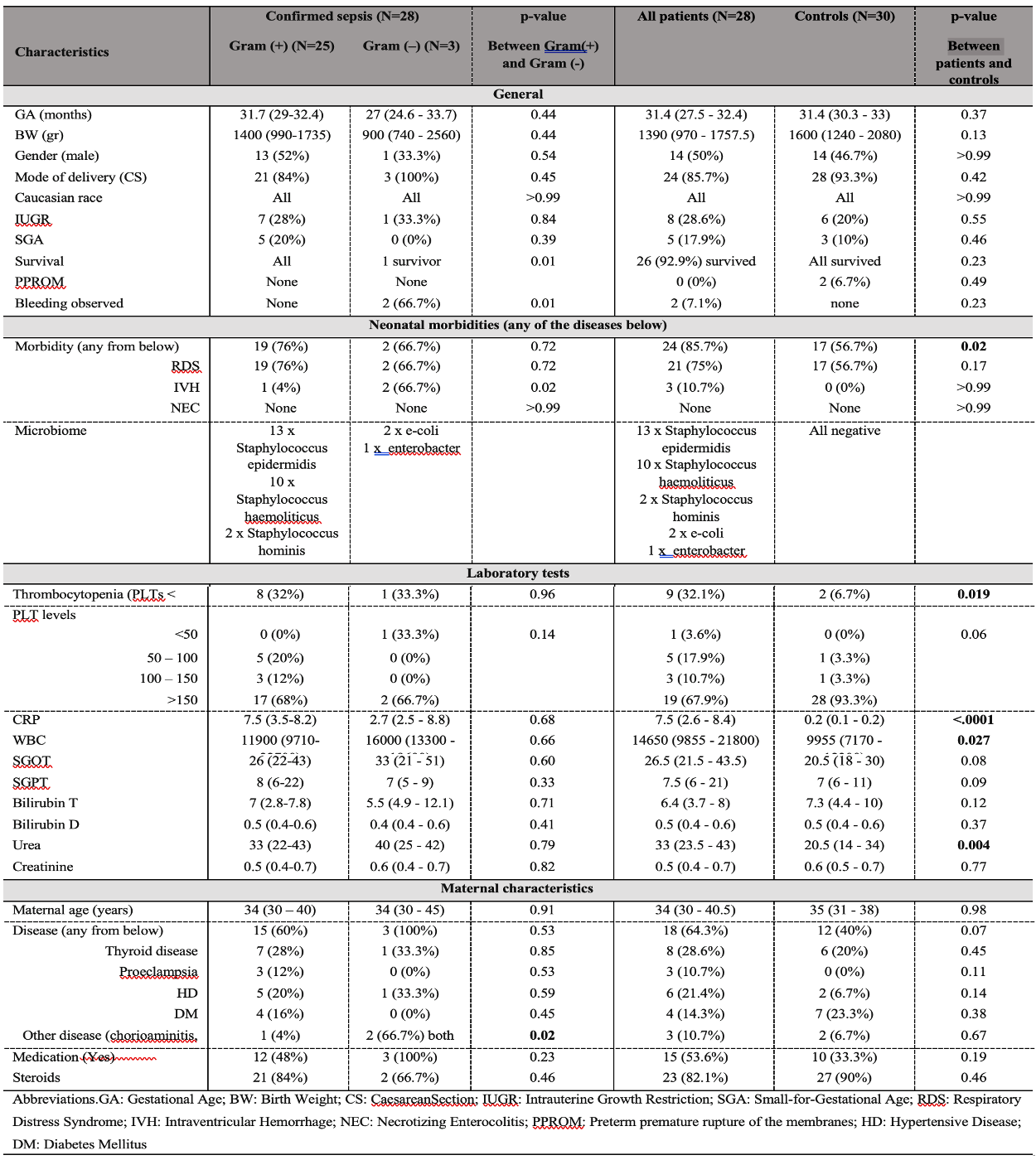
Design/Methods: We included 28 preterm neonates with sepsis born at gestational age 24 + 1 to 34 + 3 and studied in comparison to 30 healthy counterparts. Coagulation was assessed by ROTEM and platelet function by flow cytometry. The study was conducted at 3-time points, at 1st, at 2nd to 3rd, and at 5th to 7th day of sepsis for patients and at 1-time point for controls (Τable Ι).
Results: Comparison of the slopes for the fitted lines in patients and controls proved that there was no difference (p=0.9054) thus the two populations may be
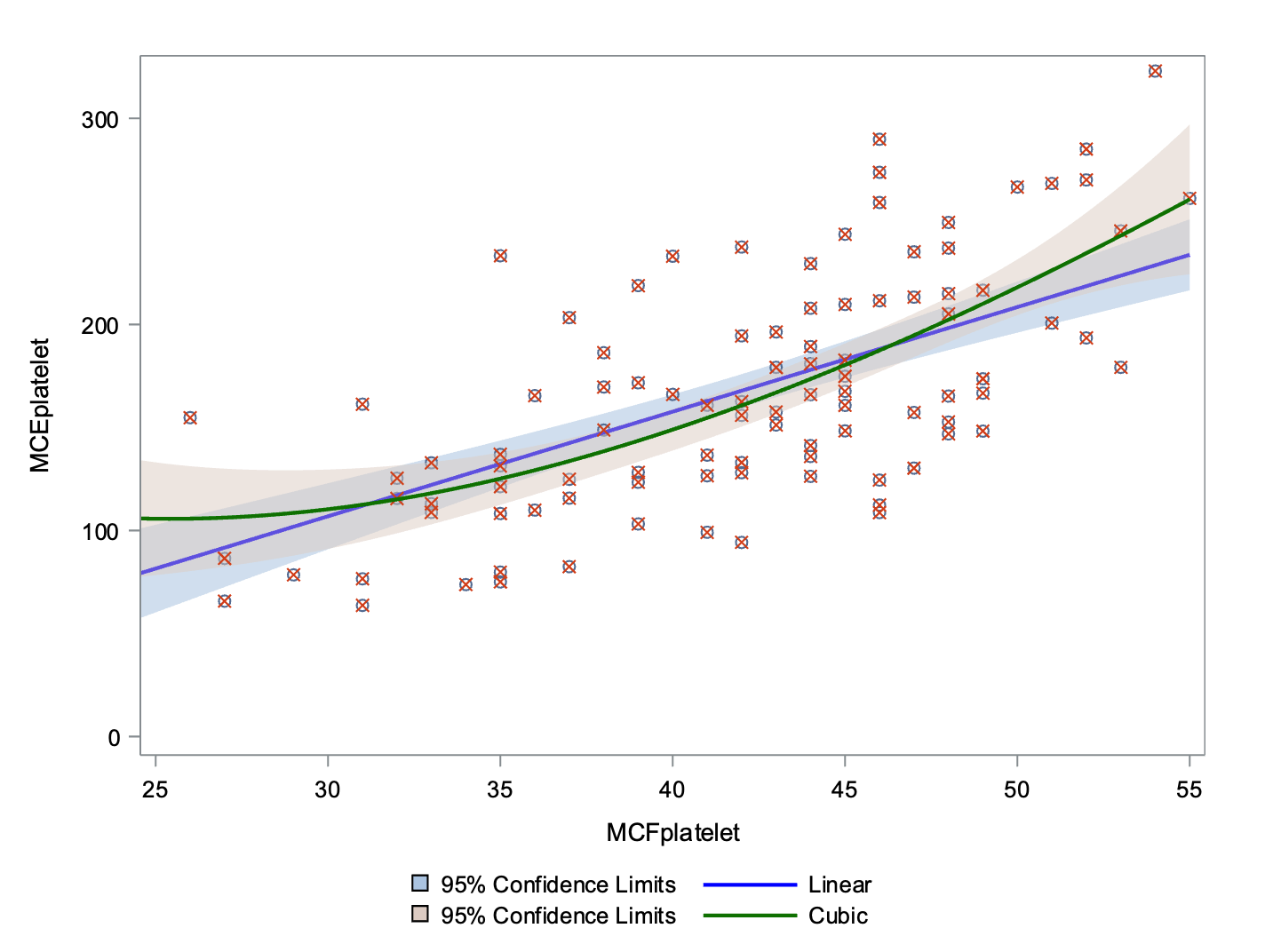
treated with a single model (Figure1). MCFplatelet and MCEplatelet were tested for association with platelet count and function in a total of 112 tests.
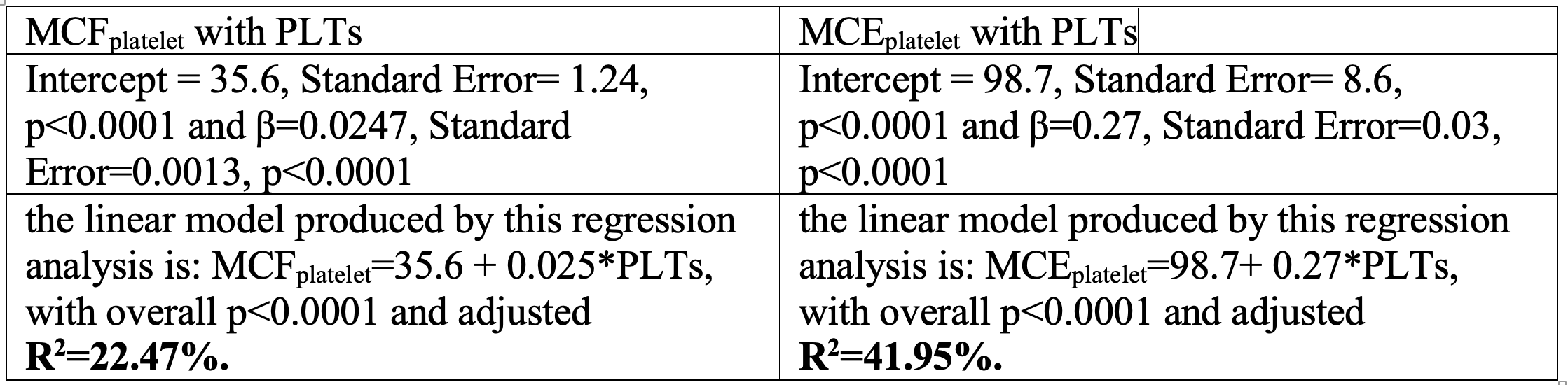
The MCFplatelet showed a low (MCF platelet =35.6 + 0.025*PLTs, with overall p<0.0001 and adjusted R 2 =22.47%) association with platelet count and function (42b receptors, R 2 =11.44% and TRAPtest, R 2 =12.69%). The MCEplatelet showed higher association (MCE platelet =98.7+ 0.27*PLTs, with overall p<0.0001 and adjusted R 2 =41.95%) with platelet count. No association was found between MCEplatelet, inactive receptors and TRAPtest (Table II, III, IV, Figure 2, 3).
Conclusion(s): In the study population (patients and controls) MCE platelet is better estimator for platelet count than MCF platelet , however fails to precisely reflect platelet function. Platelet function by flow cytometry is poorly related to MCF platelet as it is evident from the correlation coefficients and the linear regression analysis. In clinical practice, the difference in elasticity between EXTEM and FIBTEM may replace the difference in amplitude but further research and new diagnostic modalities should be performed to discriminate the contribution of platelet function to clot stability.