General Pediatrics
Session: General Pediatrics 3
343 - Changes in High Blood Pressure Screening and Detection Rates in Children and Adolescents After the 2017 American Academy of Pediatrics Clinical Practice Guideline and the COVID-19 Pandemic
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 343
Publication Number: 343.1148
Publication Number: 343.1148

Laura M. Generale, MD (she/her/hers)
Resident Physician
Wake Forest Baptist Health - Brenner Children's Hospital
Presenting Author(s)
Background: The 2017 Clinical Practice Guideline (CPG) changed detection and diagnosis of hypertension (HTN) compared to prior guidelines. While studies have reported increased prevalence of HTN in youths was due to lower HTN thresholds, there is limited evidence of how the CPG and the COVID-19 pandemic impacted blood pressure (BP) screening and diagnosis of HTN in youth in primary care settings.
Objective: Evaluate how the CPG and COVID-19 pandemic impacted BP screening and HTN detection in a resident-run primary care clinic and to assess if obesity modified these associations.
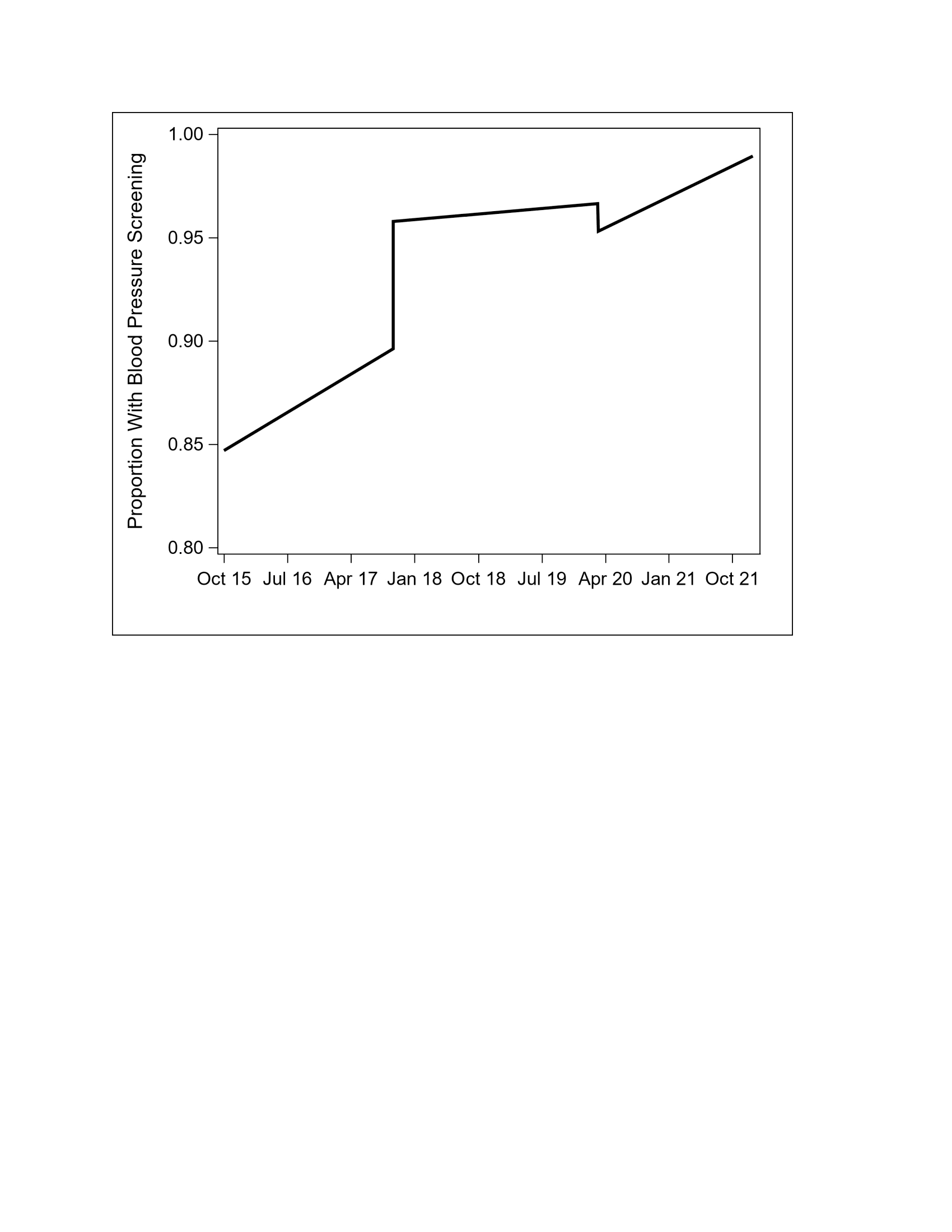
Design/Methods: Interrupted time series analysis was conducted on data collected retrospectively from the electronic health record at a single resident-run primary care clinic. Inclusion criteria were ages 3–17 years. During the Pre-CPG era (10/2015-08/2017), we evaluated all clinic visits based on inclusion criteria, while during the Post-CPG era (09/2017-02/2020) and the COVID-19 pandemic era (03/2020-03/2021), Well-Child Visits were evaluated based on inclusion criteria with month as unit of time. We collected participant age, sex, height, weight, BP, and ICD-10 codes from each visit. We calculated BP percentiles based on era-specific guidelines and BMI percentiles based on guidelines. Outcomes were the proportion of clinic visits with documented BP measurements and the proportion of documented HTN by ICD-10 codes when HTN threshold was met. We fit interrupted time series models with multivariable generalized estimating equations with a compound symmetry correlation structure, adjusted for age and sex. We also included an interaction term and stratified our models by obesity (BMI ≥95th %ile).
Results: 9,670 visits were included. Between the Pre-CPG and Post-CPG eras, the probability of BP screening and the probability of documented HTN increased significantly 0.73 to 0.92 ( < 0.001) and 0.01 to 0.05 (p 0.004), respectively. Between the Post-CPG and COVID-19 pandemic eras, the probability of BP screening decreased significantly from 0.92 to 0.15 (p 0.004), but the probability of documented HTN was not significantly different (p 0.33).
When evaluating if obesity modified the probability of BP screening or documented HTN, there was no difference in outcomes (p 0.64, 0.23).
Conclusion(s): Our data showed an increase in both the probability of BP screening and documented HTN in the clinic setting. During the pandemic, there was a significant interruption in BP screening, but no impact on the probability of documented HTN. Obesity was not found to modify the associations between eras and outcomes.
Firgure-2-PAS-abstract.jpeg
