Cardiology
Session: Cardiology 1
136 - A Community-Based Conceptual Model for Transitioning Youth with Congenital Heart Disease
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 136
Publication Number: 136.2824
Publication Number: 136.2824

Krisjon Olson, PhD (she/her/hers)
Assistant Professor
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background: Life with congenital heart disease now extends from childhood into adulthood for surviving youth. While we know that half of patients are lost in the transition from pediatric to adult care, this critical period remains understudied.
Objective: The aims of this observational, mixed methods study were to 1) document the healthcare transition experiences of young people with congenital heart disease (with and without disabilities), 2) examine the perspectives of youth, their caregivers, health care providers, and community advocates regarding barriers and facilitators to transition and 3) integrate findings into a community informed conceptual model of accessible healthcare transition.
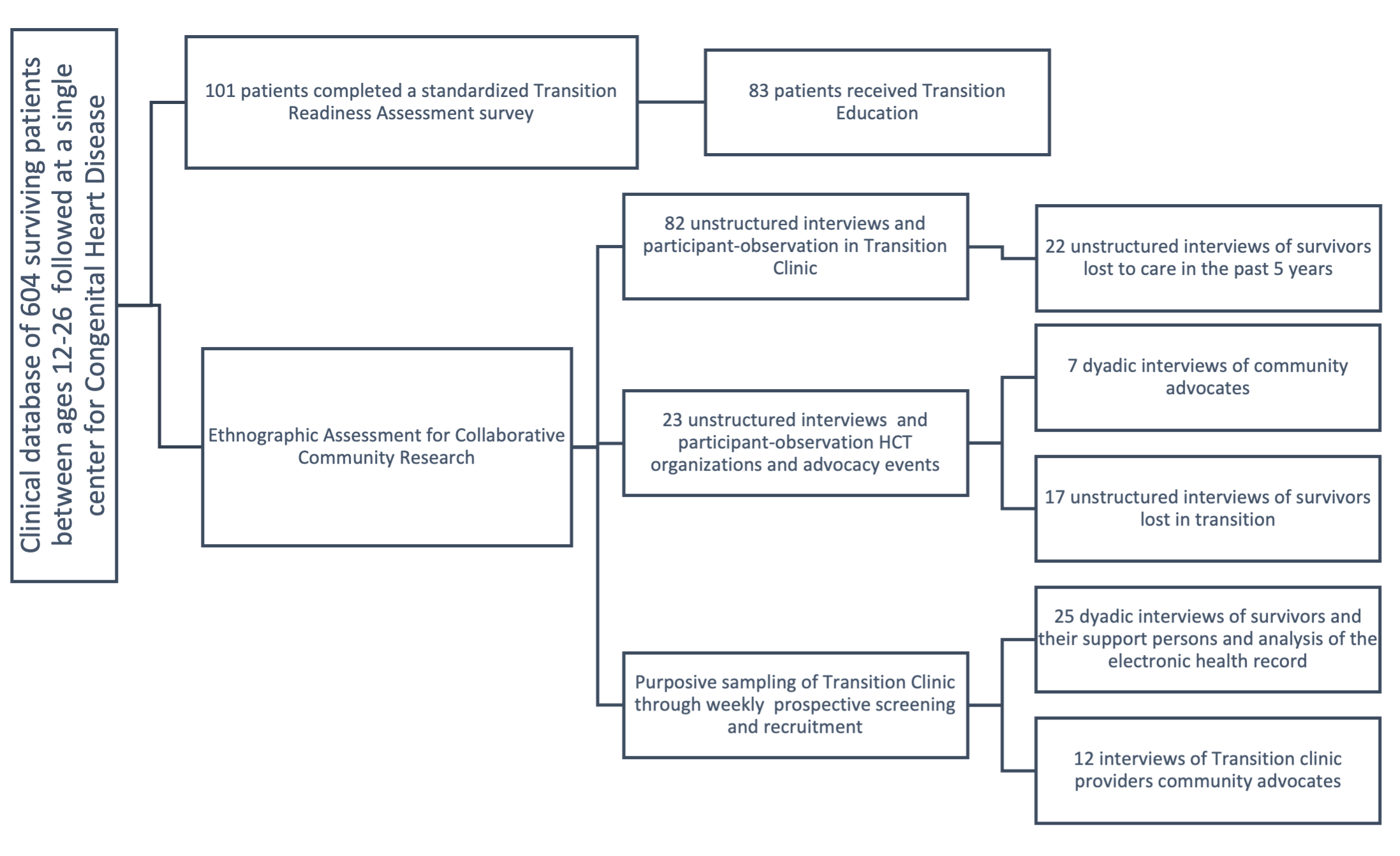
Design/Methods: Queried a clinical registry of 604 patients referred to a CHD Transition Clinic at a Midwestern academic medical center between 10/21/2021-7/31/2023 where 101 had completed standardized transition readiness assessments. A purposeful sample of the cohort ages 12-26 were stratified for disability, age, sex, gender, race, diagnosis, geography, and types of intervention received and interviewed (32 dyadic interviews with a caregiver, 22 unstructured) with text from their electronic health record analyzed. Interviews and observations of health care providers and community advocates (12 structured, 23 unstructured) were also performed.
Results: Qualitative analysis reveals transition age youth experience significant barriers (eg. a narrowing network of social support, health uncertainty, pressure to move) as well as facilitators (eg. supported decision making, adaptability, skilled advocacy) in healthcare transition. Quantitative and qualitative findings were integrated to construct a community informed healthcare transition framework for congenital heart disease. The model highlights transition as a complex process where survivors find themselves in a disability-health paradox: aging into a system of care not designed for them, where girls with disabilities were least confident in their transition to adult healthcare representing a significant gender health gap [females with disabilities (mean=4.6, SD=4.1) vs. males with disabilities (mean=7.4, SD=2.6) (p=0.028)].
Conclusion(s): Reducing the burden of CHD transition, without addressing disability, reinforces outcome disparities. A community informed, accessible, model for transition in congenital heart disease is important as we develop interventions and services to bridge gaps in care and optimize health outcomes for young survivors. Improved accessibility of health services is also critical across diverse pediatric populations.