Medical Education
Session: Medical Education 9
507 - Reproducibility of an Ongoing Neonatal Resuscitation Telesimulation Program in Level I Rural Delivery Hospitals
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 507
Publication Number: 507.2812
Publication Number: 507.2812

Misty Melendi, MD (she/her/hers)
Division Chief, Neonatology
The Barbara Bush Children's Hospital at Maine Medical Center
Portland, Maine, United States
Presenting Author(s)
Background: Simulation offers an opportunity to practice high acuity, low occurrence neonatal resuscitation program (NRP®) guidelines in rural hospitals with low birth volumes. Rural community hospitals with low birth volumes have infrequent opportunities to maintain skills needed to adequately perform neonatal resuscitation. With limited clinical opportunities, it is essential to provide ongoing training and education that allow teams to practice these skills and receive feedback on performance/areas of improvement.
Objective: Our objective was to expand our monthly pilot neonatal resuscitation telesimulation program to two additional rural community hospitals, aiming to increase delivery team adherence to the NRP® guidelines.
Design/Methods: We piloted a neonatal resuscitation telesimulation program to include three rural delivery hospitals. Delivery teams participated in neonatal resuscitation simulations with rotating staff. Monthly sessions occurred in participants’ native clinical environments with realistic team composition with 3-5 clinicians. Neonatology and simulation experts from a tertiary care center attended remotely and led a debriefing following the simulation. Sessions were video recorded for subsequent assessment of NRP® adherence.
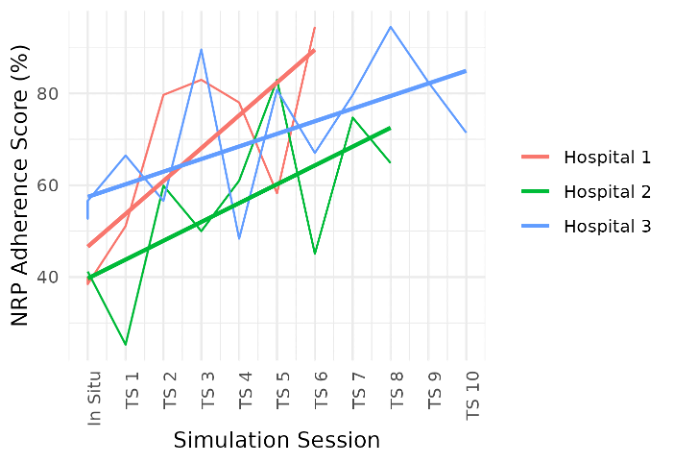
Results: Three Level I delivery hospitals participated in monthly telesimulations for a total of 6, 8, and 10 times. There were 70 clinicians who participated throughout the sessions, with some participating more than once. On average, NRP® score increased 3.5 percentage points with each training (95% CI = 1.84, 8.19; p = 0.0002) (Figure 1). Improvements were also noted in multiple NRP® subcategories including Cardiac Compressions increasing 2.282 percentage points with each training (95% CI = 1.273, 3.291; p = < 0.001), Positive Pressure Ventilation increasing 1.590 percentage points with each training (95% CI = 0.757, 2.422; p = 0.001), and Preparation/Equipment increasing 0.51 percentage points with each training (95% CI = 0.205, 0.814; p = 0.002) (Figure 2).
Conclusion(s): Improvement in NRP® adherence was noted in three rural delivery hospitals in the setting of monthly telesimulations. These results further support that our TS model is a promising method to improve neonatal resuscitation skills for rural clinicians. Our future plans include to test the generalizability of improvement in NRP adherence over time as well as to track participant attendance in order to perform a secondary analysis with unique participant identifiers as a fixed effect to understand the impact of individuals on team performance
.png)
